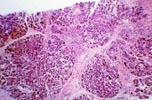
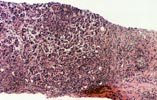

Intra-Abdominal Infections - Peripancreatic Fluid Collections A significant number of patients receiving pancreas transplants require re-laparotomy due to surgical complications. The most common reasons for re-laparotomy are intraabdominal infection and graft pancreatitis, pancreas graft thrombosis, and anastomotic leak. Need for re-laparotomy is associated with a decrease in patient and graft survival. Intra-abdominal fluid collections are treated conservatively with antibiotics and percutaneous drainage, however, abdominal exploration for drainage and debridement is often required. Needle biopsies obtained from the grafted pancreas during these surgical procedures show characteristic features. The pancreas parenchyma shows variable degrees of mixed inflammation, predominantly septal. The inflammation is composed of lymphocytes, eosinophils, neutrophils and less numerous plasma cells. A typical finding in these biopsies is the presence of dissecting bundles of active connective tissue with abundant fibroblasts. The fibrous bands run between the exocrine lobules giving the biopsy a "cirrhotic" appearance. The fibrosis becomes more pronounced as time passes if the peripancreatic infected fluid collection persists. The periphery of the acinar lobules usually shows some involvement by the inflammation. Typically, however, the acinar parenchyma shows proportionally little inflammation and acinar damage. In some cases there is pronounced interstitial edema and spotty acinar cell drop-out. The differential diagnosis in biopsies from grafts with intra-abdominal/peripancreatic abscesses is with acute and with chronic rejection. The most important piece of information useful for the differentiation from acute and chronic rejection is the history of early post-implantation peripancreatitis. The inflammation in acute rejection involves randomly the acinar parenchyma and not only the periphery of the lobules; also typically early acute rejection is not associated with fibrosis (or active septal fibroblastic proliferation). In contrast to chronic rejection in which the entire acinar structures show some degree of atrophy, in biopsies from grafts with peripancreatic infections, the central parts of the exocrine lobules do not show atrophy (only the periphery is affected by the fibrosis). Although the degree of septal fibrosis seen in biopsies from patients that
require one or more re-laparotomies may be very pronounced, these changes are
usually confined to the periphery (surface) of the graft and therefore superficial
biopsies may not represent the status of the whole organ. REFERENCES

Please mail comments, corrections or suggestions to the TPIS administration at the UPMC.
If you have questions, please email TPIS Administration. |
|