|
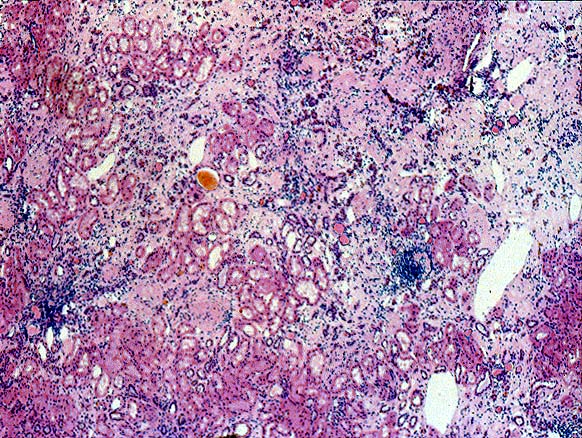
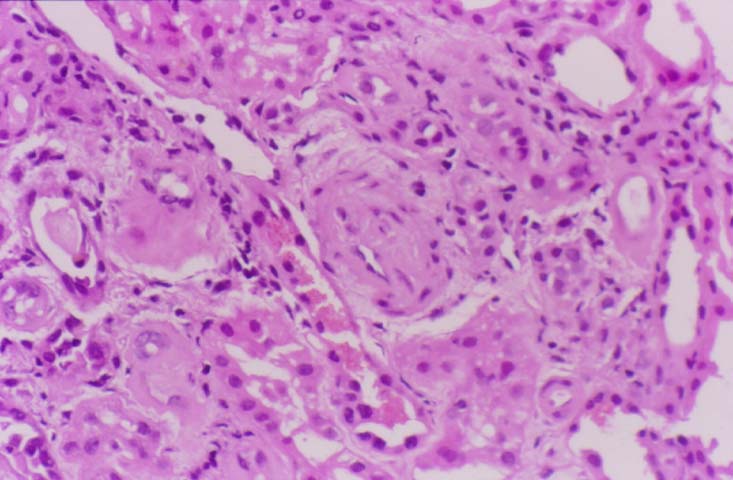
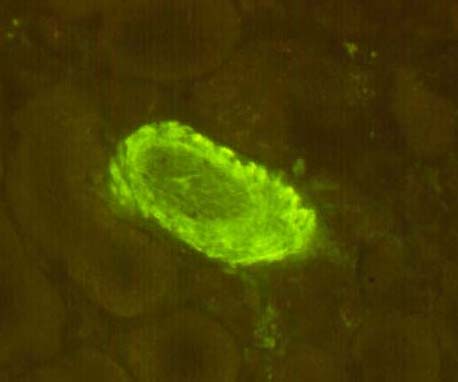
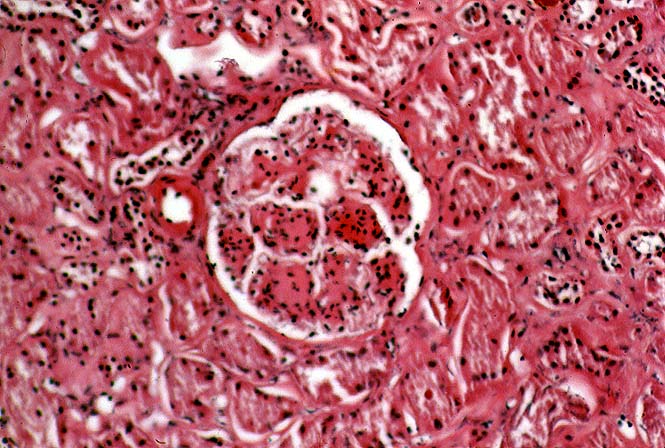
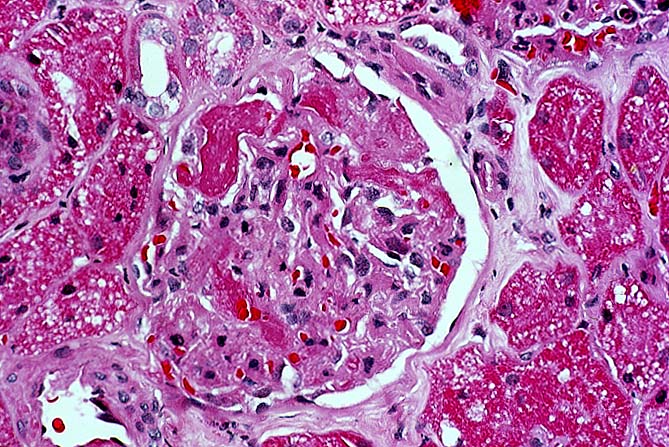
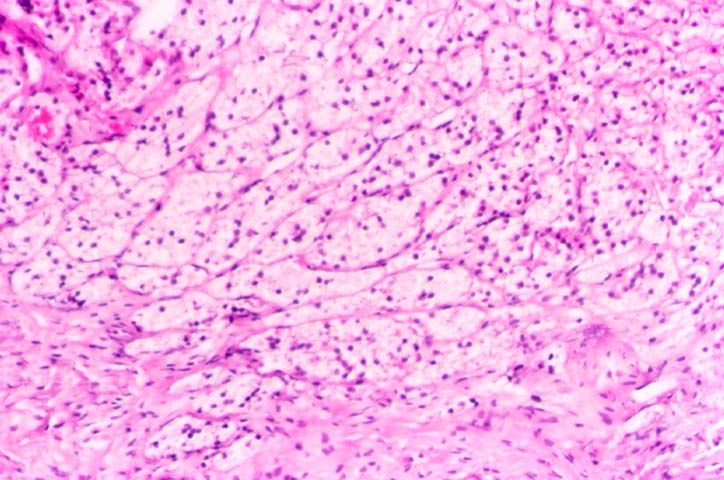
Pre-Existing Disease Some transplant centers biopsy every donor kidney for pre-existing renal disease. This is a highly desirable goal, and rapid histologic processing techniques can permit morphological evaluation by the time results of HLA typing and cross matching become available. However, other medical centers choose to biopsy only elderly donors, or donors with a history of hypertension or diabetes, and perform frozen section evaluation of biopsies prior to transplantation. Significant degrees of glomerulosclerosis, arteriosclerosis, and interstitial fibrosis can be adequately ascertained in these preparations. At Pittsburgh, kidneys with greater than 80% glomeruli patent, and only mild arteriolosclerosis and interstitial fibrosis are considered suitable for use. However, the extent of acceptable chronic changes within the donor kidney has not yet been rigorously defined. In instances where donor kidneys are not evaluated histopathologically before being used, needle biopsies performed post-perfusion, or early in the post-transplant course can document donor disease. For example, marked arteriolar thickening and hyalinosis noticed within a few days of transplant raise the possibility of donor hypertension or diabetes, particularly if the donor is young. Failure to take into account donor derived change can lead to misinterpretation of allograft biopsy findings. Thus, senile or hypertensive arteriolosclerosis may be read as cyclosporine induced hyalinosis or early chronic vascular rejection. Cadaveric donors being considered for renal transplantation occasionally show manifestations of disseminated intravascular coagulation secondary to trauma or sepsis. When renal function in the donor is satisfactory, several such kidneys have reportedly been used successfully in transplantation. Fibrin thrombi within the glomerular capillaries resolved, presumably because of an intact fibrinolytic system within the recipient. A microangiopathic anemia was transmitted to the recipients in two instances, but did not persist beyond three days. A variety of malignant neoplasms have been implanted into previously healthy people through renal transplantation. The use of donor kidneys from individuals with a current or past malignancy has lead to a recurrence of original neoplasms in approximately 50% of the recipients. This has been true whether the donor neoplasm was intra-renal or at an extra-renal location such as lung, colon, skin, breast, or uterus. For this reason, a history of malignancy should be regarded as a contraindication to organ donation. An exception can possibly be made for primary brain tumors, though, rarely even these tumors can metastasize extracranially. Sometimes a small subcapsular renal cell neoplasm is noted accidentally in the donor kidney during the harvesting procedure. It has been argued that such organs should be transplanted, if the lesion has been completely excised, and frozen section shows no overt malignancy. Nonetheless, this is a controversial issue since autopsied lesions less than 1cm in diameter and classified as "adenomas", have been known to rarely metastasize outside the kidney. References
Please mail comments, corrections or suggestions to the TPIS administration at the UPMC.
If you have questions, please email TPIS Administration. |
||||