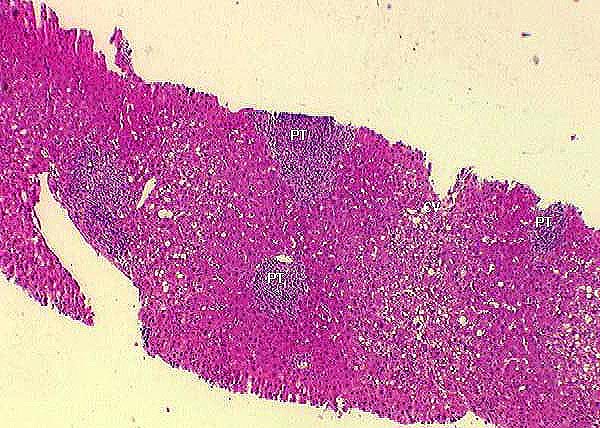
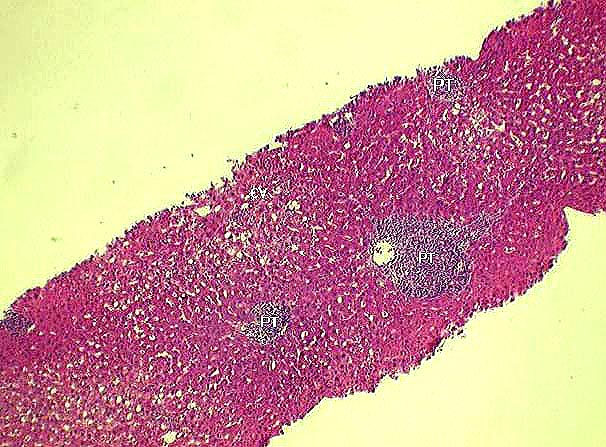
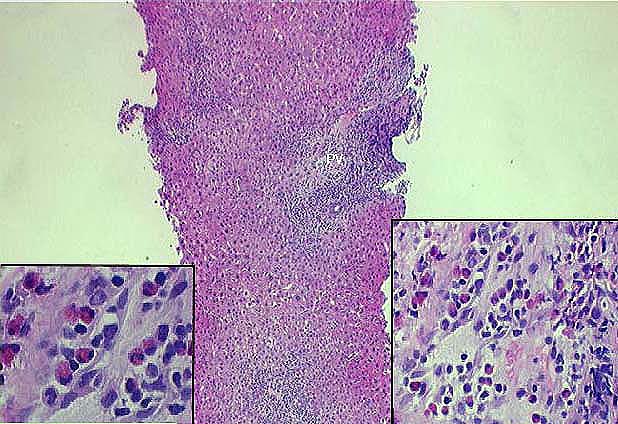
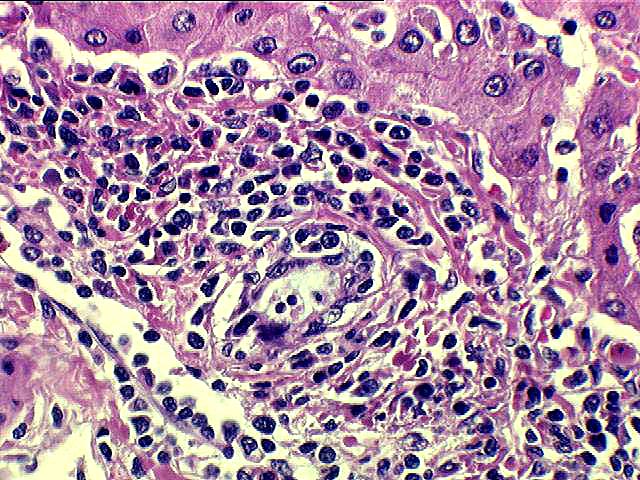
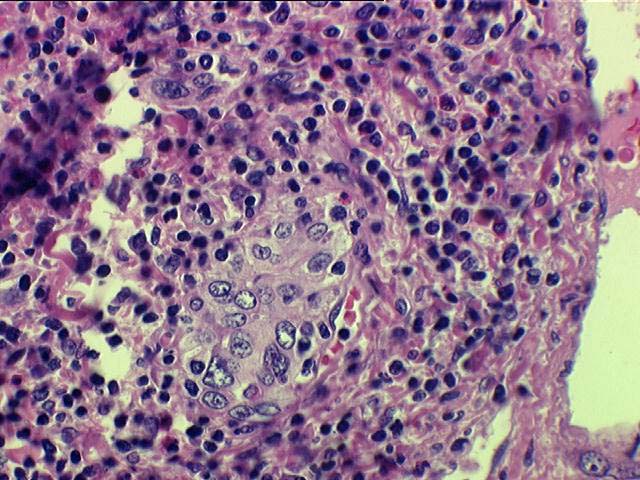
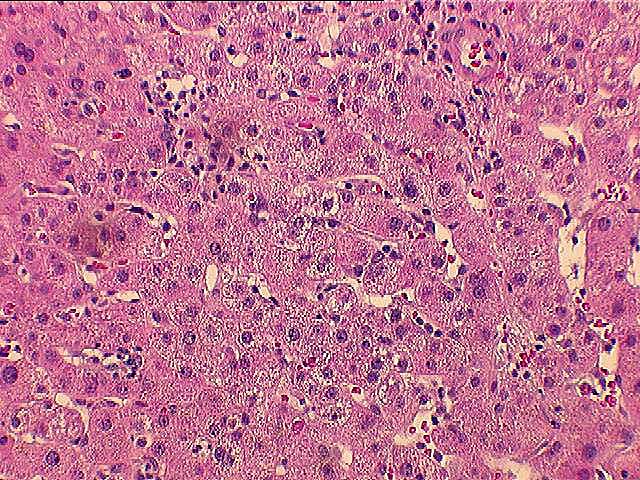
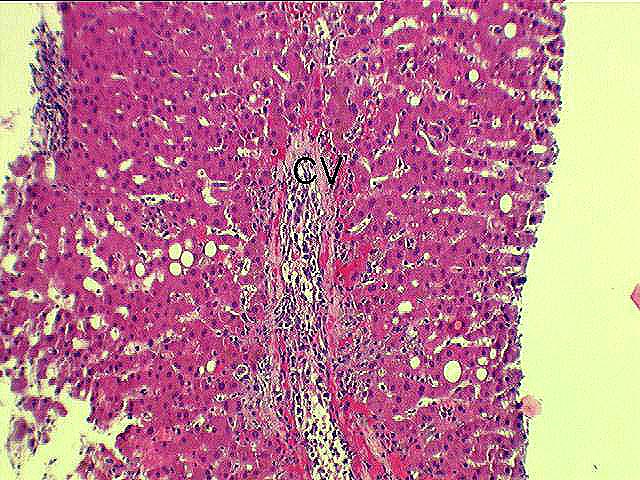
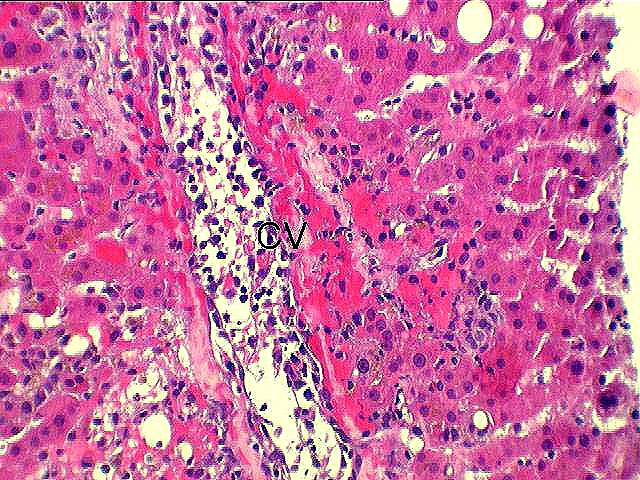
Histopathologically, the portal inflammatory infiltrate in moderate acute rejection expands most of the triads and may focally spill over into the periportal hepatic parenchyma. The severity of bile duct damage varies, but there is no perivenular (centrilobular) necrosis associated with perivenular inflammation like that seen in severe acute rejection. Most biopsies graded as "moderate" will have total RAI scores of 5 to 7.
Click here, for another example of moderate acute liver allograft rejection seen in consultation at the University of Pittsburgh.
Fortunately, most patients with moderate acute rejection will respond to treatment with increased immunosuppression in the form of increased baseline immunosuppression or pulsed corticosteroid therapy. However, compared to mild acute rejection, an increased number of moderate acute rejection episodes will be "corticosteroid-resistant" and require treatment with monoclonal antibodies.
|
|
|
|