Patients with severe acute rejection, will almost invariably show elevations of liver injury tests and there will be other symptoms of acute rejection, previously discussed , which include allograft enlargement and tenderness, and decreased quantity or quality of bile flow. These are often accompanied by fever and leukocytosis, simulating a systemic infection.
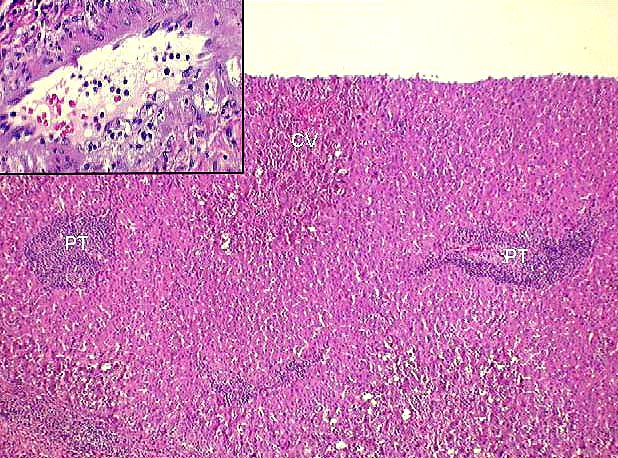
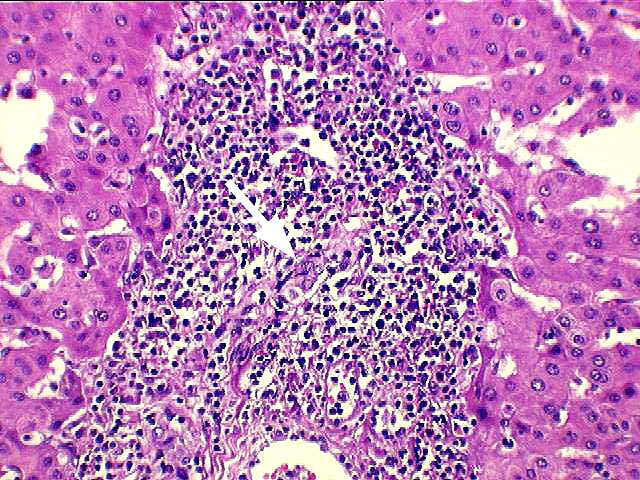
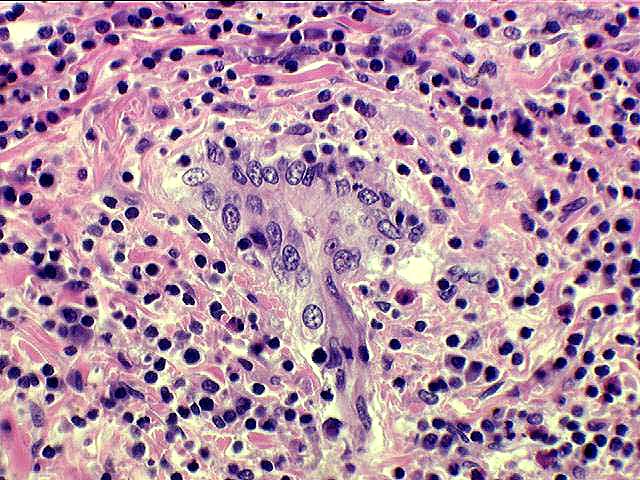
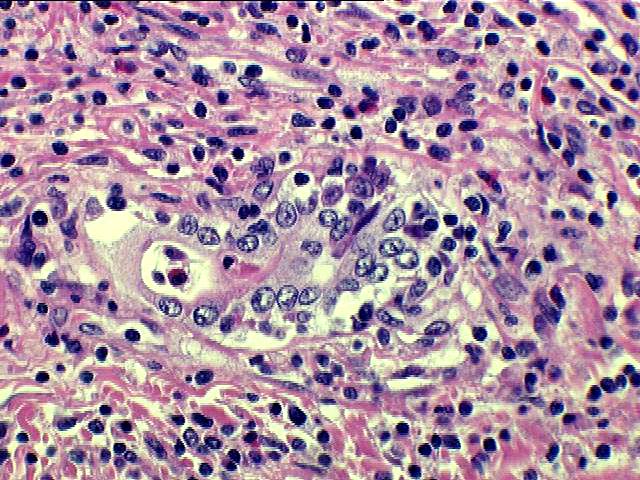
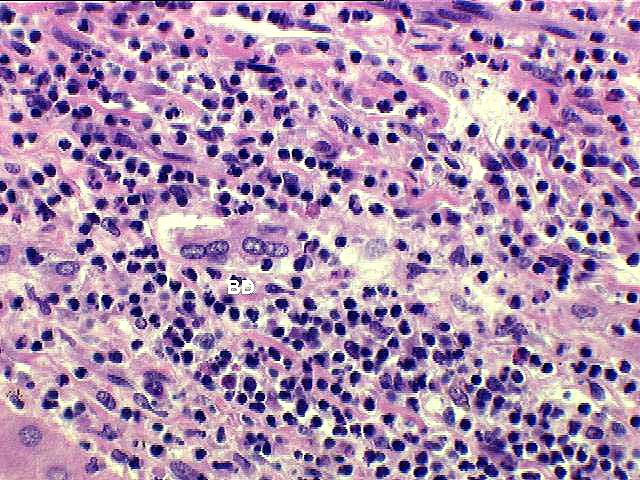
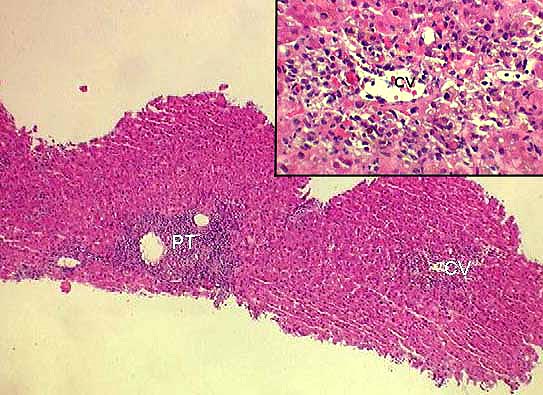
Histopathologically, severe acute rejection shows brisk portal inflammation that expands most of the triads and often extends into the periportal hepatic parenchyma, similar to moderate acute rejection. More importantly, there is inflammation in and around the connective tissue sheath surrounding the terminal hepatic venules, which extends out into the perivenular parenchyma and is associated with perivenular hepatocyte necrosis. In fact, the combination of perivenular inflammation and associated necrosis is the critical lesion used to recognize severe acute rejection. The associated mononuclear perivenular inflammation helps to distinguish ischemia-induced perivenular necrosis from that seen with severe acute rejection. In some of these cases, the accompanying bile duct damage is severe, with disruption of the ductular basement membrane and even partial destruction of the duct, recognized by the presence of a few biliary epithelial cells. This can quickly lead to bile duct loss, or chronic rejection.
It should be stressed that the perivenular necrosis and inflammation of severe acute rejection must occur in combination with the typical portal inflammation and duct damage characteristic of acute rejection. Perivenular necrosis and inflammation alone can be seen with more mild forms of rejection, but these occur in association with none or mild portal portal inflammation and none or mild bile duct damage. Click here for a typical example of a consultation case with perivenular inflammation and damage, in association with mild portal tract changes.
Once a grade of severe rejection has been established, the pathologist can ascribe a Rejection Activity Index(RAI) score to the biopsy. In the vast majority of cases, the total score will range from 7 to 9 and the venular inflammation score is by definition a "3".
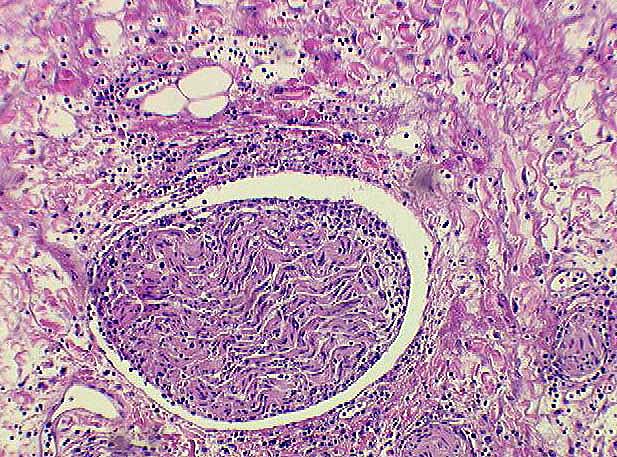
Rarely, arteritis can be seen in a needle biopsy with severe acute rejection. Although this is almost always an ominous finding in allografts with acute rejection, arteritis most commonly affects larger perihilar branches of the hepatic artery that are not sampled in needle biopsies. Because of the infrequent sampling and difficulty in reproducing the histopathological reading of arteritis, it was decided by an international panel of experts to exclude it from the grading system at this time.
Unfortunately, an increased percentage of patients with severe acute rejection will require treatment with monoclonal antibodies to control the episode, or will undergo retransplantation or die of rejection, compared to the lower grades of acute rejection.
|
|
|
|