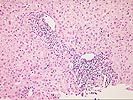
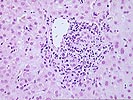
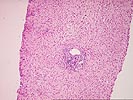
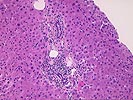
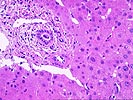
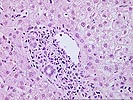
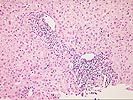
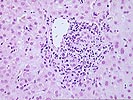
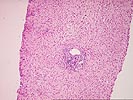
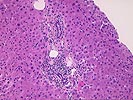
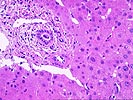
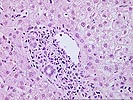
The grading of acute liver allograft rejection already presupposes that the diagnosis has been established. The diagnosis, in turn, is based on the following findings: 1) a mixed but predominantly mononuclear portal inflammation, containing blastic (activated) lymphocytes, neutrophils and frequently eosinophils, 2) bile duct inflammation/damage, and 3) subendothelial inflammation of portal veins or terminal hepatic venules. At least two of these three features are required for the histopathological diagnosis of acute rejection. Biochemical evidence of liver damage manifest as increased results on tests for liver injury, usually elevation of serum g-glutamyl transpeptidase and alkaline phosphatase activities, are also frequently present. The diagnosis is strengthened if > 50% of the ducts are damaged or if unequivocal endotheliitis of portal vein branches or terminal hepatic venules can be identified(1,2).
In some case, particularly early after transplantation, a rejection-type portal may be present, but the overall findings do not meet the minimal histopathological criteria needed to establish the diagnosis with certainty. In such cases, the grade of "indeterminate" should be used. If should be emphasized however, that the use of the indeterminate category be restricted to cases that have minor degreees of cellular infiltration that could possibly represent low grade rejection, but fail to meet the minimal diagnostic criteria, listed above. "Indeterminate" should not be used for cases in which one is unsure whether the inflammation is related to some other condition, such as chronic hepatitis C. Above are some examples of indeterminate for acute rejection(2). Most biopsies graded as "indeterminate" will have total RAI scores of 3 or less.