Herpes Simplex Types I and II and Varicella-Zoster Viral Hepatitis
Most herpes simplex(HSV) infections after liver transplantation are oral or genital reactivations of pre-existing infections(1). As with other "opportunistic" viruses significant disease is more common in recipients who are seronegative before transplantation and in patients who are heavily immunosuppressed with monoclonal antibodies(1, 2). Both subtypes of HSV(type I and II) and Varicella-Zoster (VZ) have been identified as causes of liver allograft hepatitis(2-5). Liver involvement has been seen as early as three days post-transplant but may occur anytime thereafter. The clinical presentation of patients with hepatitis has included fever, vesicular skin rashes, fatigue and body pain, combined with serologic evidence of liver injury. If HSV hepatitis goes unrecognized, it may rapidly lead to submassive or massive hepatic necrosis, hypotension, disseminated intravascular coagulation and metabolic acidosis(2). Fulminant cases usually occur in patients without evidence of prior humoral immunity. Early recognition using needle biopsy sampling is particularly crucial since effective medical therapy is available(2).
Histopathologic Findings
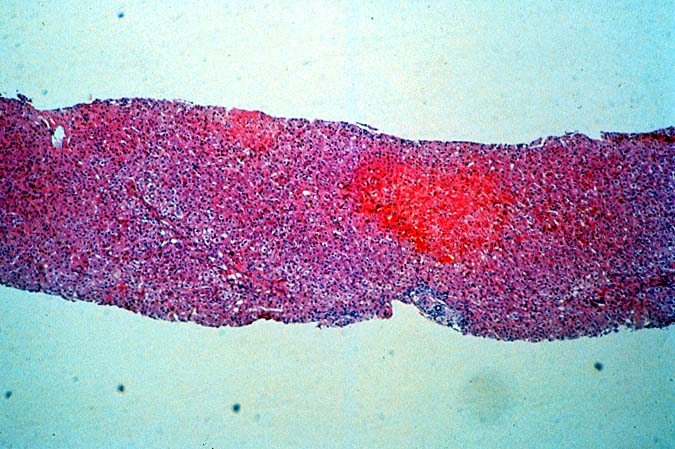
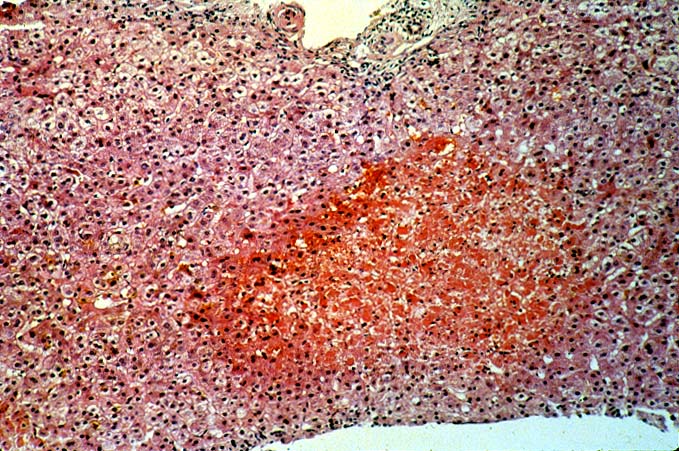
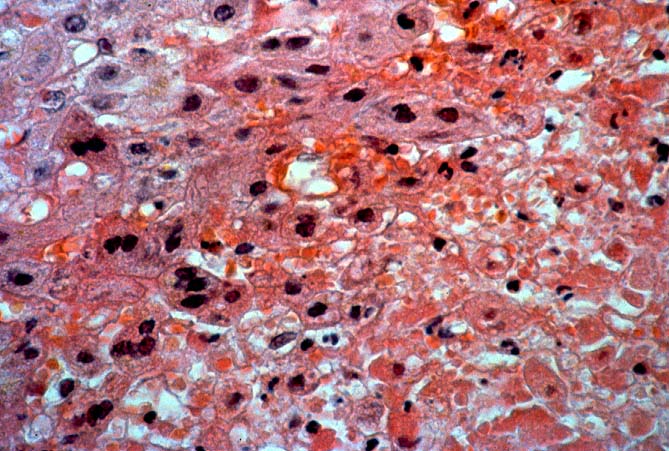
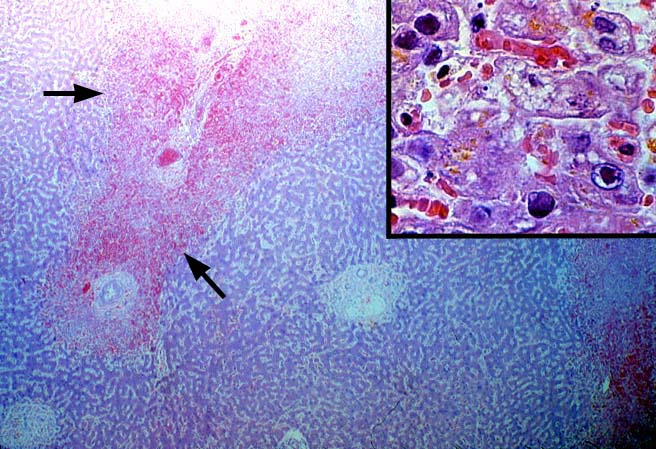
The classical pattern of injury associated with HSV/VZ hepatitis is circumscribed areas of coagulative-type necrosis showing no respect for the lobular architecture(2-5). Ghosts of hepatocytes, intermixed with neutrophils and nuclear debris are seen in the center of the lesions. More viable hepatocytes at the periphery may be slightly enlarged and contain "smudgy", or ground glass nuclei or characteristic Cowdry type A eosinophilic inclusions. The extent of liver involvement has been separated into two histopathologic patterns, localized and diffuse, with the former carrying a better prognosis(2). However, the extent, or pattern of involvement, may be more related to speed with which the diagnosis was established; the level of immune competence and evidence of prior immunity, than to differences in the viral biology.
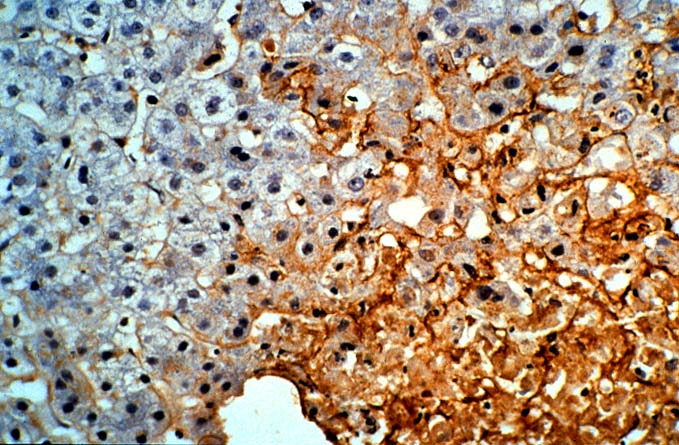
Multi-nucleate cells are occasionally present, but not infrequently, no changes diagnostic of HSV or VZ will be detected on the H & E slide. In such cases, immunoperoxidase stains for HSV antigens can be confirmatory. Some antibody preparations used to detect HSV subtypes show considerable cross reactivity making it difficult to separate HSV I from HSV II using immunohistochemistry. Regardless of the presence or absence of inclusions, we have not been able to reliably separate HSV from VZ on the H & E slides alone. This usually requires clinical correlation and the use of anti-HSV and anti-VZ monoclonal antibodies to identify specific viral antigens.
Differential Diagnosis
It can be very difficult to separate the edge of a focal infarct from the periphery of a necrotic HSV lesion. Global ischemic insults usually cause zonal hepatocyte necrosis or damage. The most obvious distinction between HSV/VZ and ischemia is that inclusion bodies are present in HSV or VZ hepatitis and absent at the periphery of an infarct. However, even in cases of HSV/VZ hepatitis, unequivocal viral inclusions may not be present; only cells with a smudged nuclear chromatin will be found. In such cases, it is our policy to over-diagnose HSV hepatitis on the H&E slides alone, since without the highly effective anti-viral therapy, HSV/VZ hepatitis can rapidly disseminate, causing liver failure and death.
Distinguishing HSV/VZ hepatitis from CMV hepatitis is occasionally problematic in cases where there is a paucity of necrosis and multinucleated cells with obvious viral inclusions are present. In such cases, it is important to carefully look for areas of ischemic-like necrosis in all sections, because CMV rarely if ever causes confluent hepatocyte necrosis. In addition, CMV infected cells will occasionally contain both nuclear and cytoplasmic inclusion, whereas the inclusions of HSV are exclusively nuclear.
Lastly, in some cases it may be difficult to distinguish HSV/VZ from adenovirus hepatitis, because both can cause punctate or circumscribed areas of confluent hepatocyte necrosis. Careful examination of the nuclear inclusions in such cases will often be helpful. In addition, adenovirus is often associated with a vaguely granulomatoid response or macrophages infiltration, whereas HSV/VZ hepatitis lesions usually contain few mononuclear cells. Instead, neutrophils usually surround the periphery of the necrotic zones. In the end, clinical correlation and immunoperoxidase staining to identify specific viral antigens will establish the diagnosis with certainty. Adenovirus is more typically seen in the pediatric population, presumably since most adults already have protective immunity.
REFERENCES
|
|
|
|