ADENOVIRAL HEPATITIS
Introduction and Pathophysiology
Adenoviral infection and disease after liver transplantation is
largely limited to the pediatric population (1-3), although it
occasionally can be seen in adults. The difference in frequency
between the two different age populations is presumably related
to prior protective immunity, much like the situation seen with
CMV, EBV and the other "opportunistic viral infections..
Viral subtypes 1, 2 and 5 have been isolated from the lung, gastrointestinal
tract and liver in patients with fever, respiratory distress,
diarrhea, and liver dysfunction(1-3). The onset of symptoms attributable
to adenoviral infection usually occurs between 1 and 10 weeks
after transplantation. Tissue biopsies and histopathological analyses
are used to ascertain the diagnosis. Liver involvement with frank
hepatitis is most often caused by subtype 5. However, viral subtypes
2, 11 and 16 have been associated with hepatitis in the general
population and therefore, could be expected to behave similarly
in liver allograft recipients(1-3).
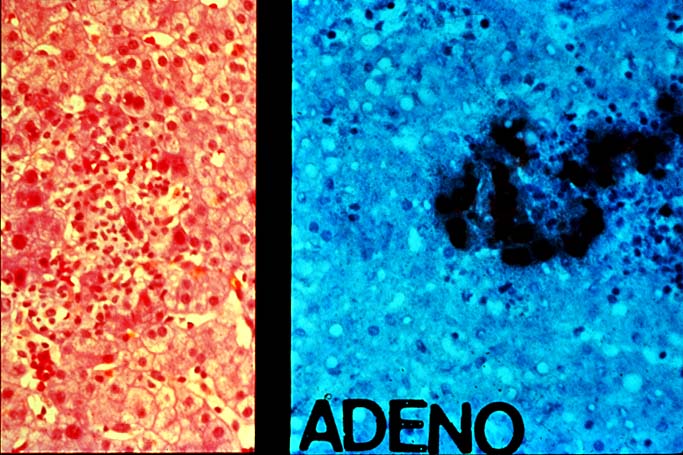
Histopathologic Findings
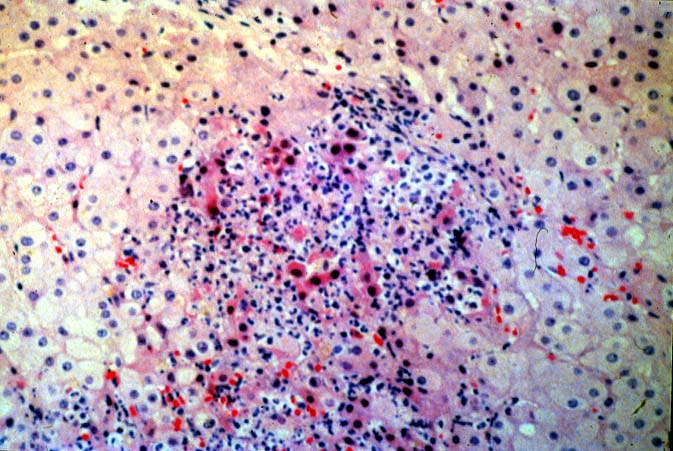
Some experience is usually required to establish the diagnosis
with certainty and therefore, immunohistochemical confirmation
of the presence of viral antigens can be very helpful. The most
characteristic changes on routine light microscopy, are the presence
of "pox-like" granulomas, consisting almost entirely
of macrophages, which are spread randomly throughout the parenchyma,
encompassing small groups of necrotic hepatocytes (1-3). In other
cases, the granulomatoid collections of macrophages are replaced
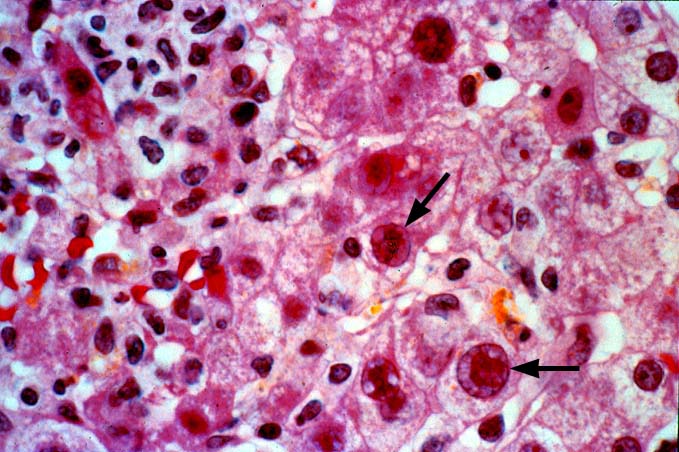
by necrosis that can be rather extensive. Adenoviral inclusions,
when identifiable, are often located near the edge of the necrotic
zones and/or granulomas. They are characterized by a crowding
of chromatin towards the nuclear membrane, imparting a muffin-shape
appearance to the nucleus. Immunohistochemical staining are confirmatory.
Portal inflammation is variably present, but subendothelial inflammation
of portal and/or central veins and bile duct damage are not usually
seen.
Differential Diagnosis
The histopathologic differential diagnosis includes deep fungal or mycobacterial infections, CMV and HSV-VZ, ischemic necrosis, and non-specific granulomatoid collections of macrophages, which are not uncommon in liver allograft biopsies. Obvious adenoviral inclusions clinch the diagnosis. However, inclusions are not always identified or easily distinguished from other types of viral inclusions. The granulomas associated with adenovirus consist almost entirely of macrophages, are much larger than the "micro-granulomas" of CMV, and multinucleated giant cells are rare. In contrast, CMV causes cytomegaly of the involved cell, and CMV can produce both eosinophilic intranuclear inclusions surrounded by a clear halo, and basophilic or amphophilic small cytoplasmic inclusions. In contrast, Adenovirus usually does not cause significant cytomegaly. In addition, the infected nuclei are "smudgy-appearing" and there are no cytoplasmic inclusions. The hepatocyte necrosis associated with Adenovirus is generally less than that seen with Herpes Simplex or Varicella-Zoster hepatitis. However, in other cases, the two(Adenovirus and Herpes Simplex or Varicella/Zoster) can appear quite similar.
The zones of ischemic necrosis seen with vascular compromise of one sort or another, can appear similar to the necrosis seen with Adenovirus and HSV-VZ. However, in the former, the necrosis almost always shows a lobular or zonal distribution whereas in the latter, the distribution of necrosis is apparently random. In addition, virally infected cells are usually absent in ischemic damage.
Non-specific granulomatoid collections of macrophages are not infrequent in liver allograft biopsies. However, there usually is little other evidence of tissue damage and the clinical profile is not typical of a viral syndrome. In addition, typical inclusion bodies are not seen.
A not insignificant number of cases will remain where significant
pathological changes are seen, but inclusion bodies are not present,
or the pathologist is unsure. In such cases, information gained
from ancillary studies can provide useful information. For example,
microbiologic cultures of the biopsy and negative special stains
for granuloma-causing organisms make fungal and mycobacterial
infections less likely. The clinical syndrome and findings provide
additional useful information. Finally, the presence of Adenoviral
antigens confirmed by immunohistochemical staining is confirmatory.
REFERENCES
|
|
|
|