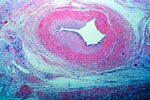
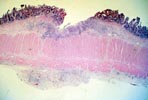

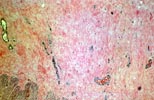
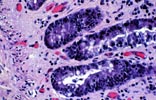
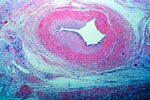
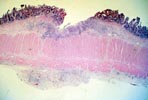

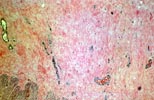
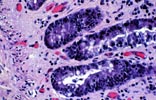
The common clinical presentation of chronic small bowel allograft rejection is persistent diarrhea with non-healing mucosal ulceration, often following repeated bouts of acute rejection. Endoscopically, the mucosal folds are effaced, the bowel appears firm and fibrotic, and focal ulcers are often seen. The primary histologic feature, as in other solid organ grafts, is obliterative arteriopathy. The larger arteries within the bowel serosa and muscularis propira are most severely affected. Unfortunately, however, these vessels are not routinely sampled by biopsy specimens, although they may be evaluated with angiography. Other features are less specific, but are more apt to be found in mucosal biopsies. These include discrete ulcers accompanied by mucosa showing evidence of prior injury and regeneration (disordered and irregular crypt and villus architecture, epithelial adenomatous changes, mucosal fibrosis, granulation tissue) together with ongoing crypt cell apoptosis. The submucosa can be severely fibrotic, producing a thickened, unyielding bowel wall resembling Crohn's disease.
|
|
|
|