On the tenth post-op day, the clinical signs and the changes of the labor values raised the question of the acute rejection. In that occasion, the patient was given steroid SHOT -- 500 mg methylprednisolone, intravenously, three times. The parameters of liver functions (except serum bilirubin) became better.
Mental status is comatous still now. The EEG signs became slightly better. From the cystic drain came less, and more light color bile.
During the observation, the microbiologic findings were not seriously abnormal. There was no real sign of sepsis or bacterial, mycotic, or viral infection. The immunosuppressive treatment contains cyclosporine A (the dosage is followed the serum level), and methylprednisolone 25 mg/day. Review of outside material.
Previous Biopsies on this Patient:
None
TPIS Related Resources:
Liver
Allograft Rejection Grading
Liver
Transplant Topics
(1 HE, 1 Picro, 1 PAS, 1 PAS/D, 1 Iron)
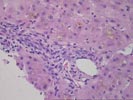
The normal lobular architecture is
mildly distorted because of mild portal expansion because of focal duct and
cholangiolar proliferation and a mild mixed inflammatory cell infiltrate,
containing occasional eosinophils. No definite portal or central venulitis is
seen, and only focal minimal duct damage is seen. Most of the other ducts are
normal in appearance.
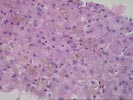
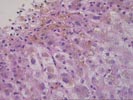
The most striking changes are in the lobule. There is panlobular hepatocanalicular cholestasis and perivenular hepatocellular dropout. Spotty acidophilic necrosis of hepatocytes is also seen.
Assuming that the hepatic vasculature is patent, the changes appear to be largely attributable to ischemia/preservation injury. The perivenular hepatocyte dropout can be caused by a previous episode of hypotension, either in the donor or recipient. The focal eosinophilia is suggestive of an early component of acute rejection, but the changes are not florid enough at this time to warrant a definitive diagnosis. The clinical profile including the marked elevations of the LDH, ALT and AST on day 1, which gradually normalized over the next two weeks, while the serum bilirubin, which was initially low then began to rise, is typical for an ischemic/preservation injury syndrome. However, if serum bilirubin levels continue to rise, or fail to slowly decrease over the next several weeks, other causes of pure cholestasis, such as adverse drug reaction and sepsis, or superimposed rejection should be considered. In addition, recurrence of viral hepatitis type C 3-4 weeks after transplantation is quite common. Re-biopsy at that time may be helpful. I look forward to any follow-up in this case.