Per referral report, the patient is a 49 year-old female who was transplanted in 1992. The diagnosis was cirrhosis secondary to autoimmune hepatitis with a suspicion of variant PBC. Review of outside material.
PART 2: LIVER ALLOGRAFT, NEEDLE BIOPSY -
PART 3: LIVER ALLOGRAFT, NEEDLE BIOPSY -
Previous Biopsies on this Patient:
None
TPIS Related Resources:
Liver Allograft Rejection Grading
Liver Transplant Topics
Their Part 1 (3 HE, 1 Hepatitis B surface antigen, 1
Hepatitis B core antigen).
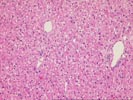
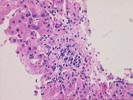
The normal lobular architecture is distorted by centrilobular
hepatocellular necrosis with dropout and perivenular inflammation
consisting of lymphocytes, plasma cells and pigmented
macrophages. The portal tracts are also minimally expanded
secondary to a very mild focal inflammatory cell infiltrate.
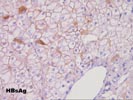
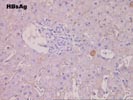
Throughout the remainder of the lobule, there is minimal disarray but ground glass hepatocytes are easily recognized. Special stains for hepatitis B surface antigen are positive in a diffuse surface membrane expression as well as the classical intracytoplasmic inclusions. Stains for hepatitis B core antigen are negative with an appropriate positive control included.
Their Part 2 (3 H&E, 1 Hepatitis B core antigen, 1
Hepatitis B surface antigen)
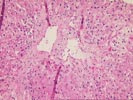
The normal lobular architecture is intact and greater than 10
portal tracts are identified, mostly of which are free of
inflammation. No bile duct damage nor loss are seen. There
continues to be mild perivenular hepatocellular dropout,
congestion and hemorrhage, but now only a minimal inflammatory
cell infiltrate. Occasional pigmented macrophages are seen.
Compared to the previous biopsy the centrilobular regions have
greatly improved.
Ground glass hepatocytes continue to be easily recognized. In addition, there is periportal hepatocellular swelling, strongly suggestive of recent, high dose, corticosteroid therapy.
Stains for hepatitis B surface antigen are positive in a cytoplasmic inclusion and diffuse surface membrane pattern. Stains for hepatitis B core antigen continue to be negative with an appropriate positive control.
Their Part 3 (3 HE, 1 Hepatitis B core antigen, 1
Hepatitis B surface antigen)
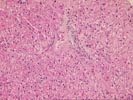
The normal lobular architecture is distorted because of mild
portal expansion and mild to moderate perivenular hepatocellular
dropout, mild fibrosis, congestion and inflammation. In fact,
the perivenular changes are predominant.
A few of the portal tracts show a mild mononuclear inflammatory cell infiltrate and focal ductular reactivity. Mild focal interface activity is appreciated. However, the most striking changes are in the lobule, predominantly in the perivenular regions which show the changes mentioned above. In addition, there continuous to be numerous ground glass hepatocytes identified.
Stains for hepatitis B core antigen continue to be negative with the appropriate positive control. Stains for hepatitis B surface antigen show a cytoplasmic inclusion pattern.
Overall, the histopathological changes suggest that more than one insult is contributing to the liver injury. However, the predominant process is central venulitis with perivenular hepatocellular dropout, congestion and focal fibrosis. In our opinion, this perivenular reaction represents an acute rejection reaction and will respond to increased immunosuppression.
There is however, very mild focal interface activity and mild portal expansion. This could be either related to a mild component of chronic viral hepatitis type B or recurrence of the autoimmune syndrome, as per clinical history. The latter is favored. The continued absence of hepatitis B core antigen staining in the biopsy suggests a non-replicative form of the virus. This may be related to antiviral chemotherapy and/or integration of the viral genome and defective viral replication. Nevertheless, the rejection reaction is predominant at this time. I look forward to any follow-up in this case.