An excisional biopsy of a supraclavicular lymph node turned out to be a localized area of necrosis within the subcutaneous tissue. There is no real granuloma formation or evidence of a pre-existing lymph node. All cultures have been negative. No evidence of PTLD. He has been imperically treated with numerous antibiotics, anti-fungal agents, and anti-tuberculous agents--all without result. Currently, his serum chemistries are TB 15.9; AP 255; GGT 345; AST 340; ALT 276, ALB 2.9; PT 13.8. His immunosuppression has been discontinued. Review of outside material.
Previous Biopsies on this Patient:
NONE
TPIS Related Resources:
Liver
Allograft Rejection Grading
Liver
Transplant Topics
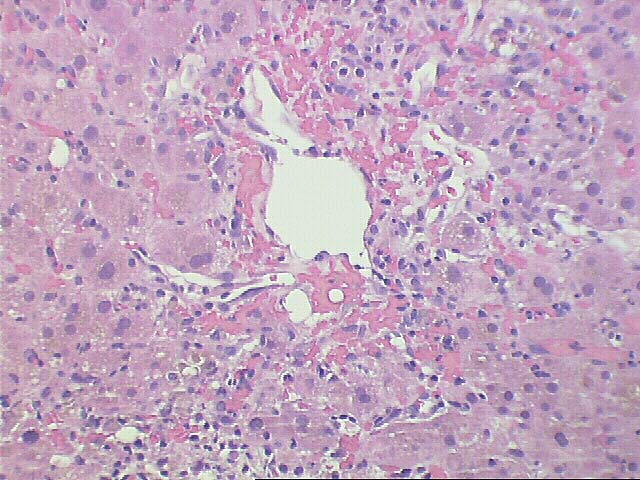
The normal lobular architecture is distorted by portal expansion because of edema and focal hemorrhage. There is also a mild focal, predominantly mononuclear portal infiltrate and focal bile duct infiltration and damage are identified.
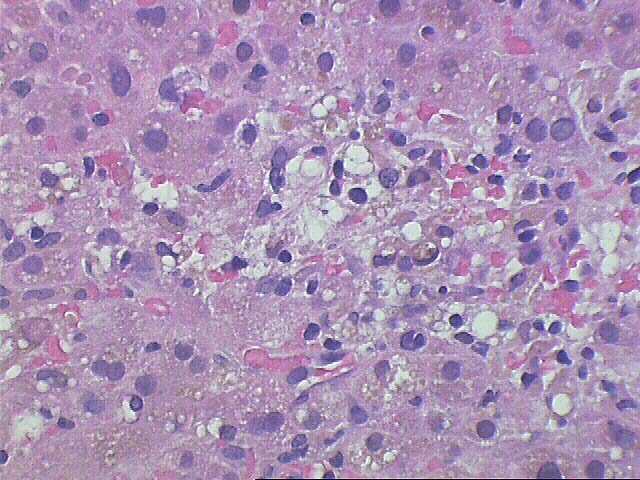
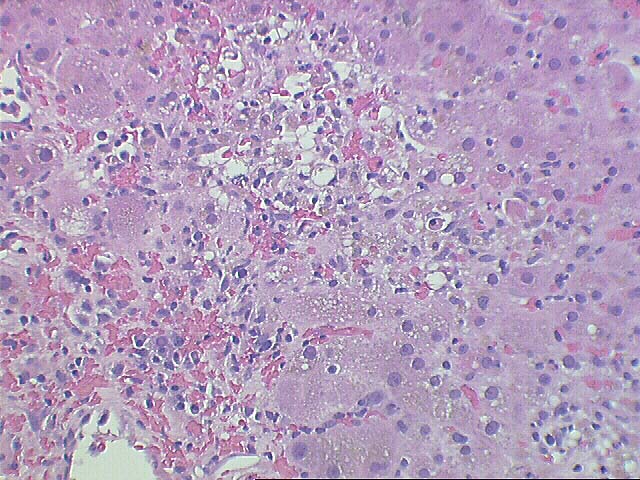
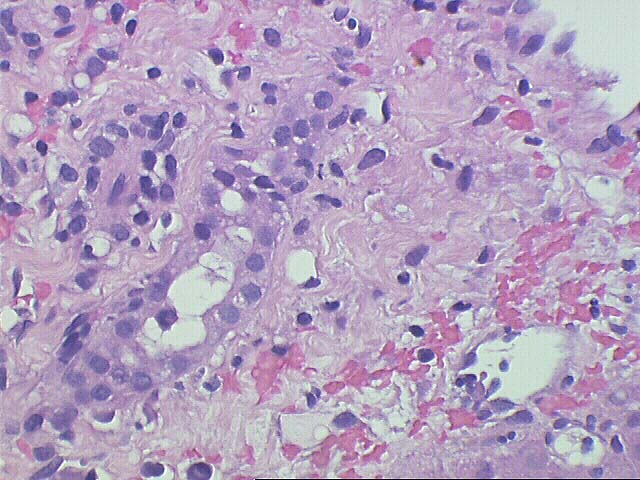
The most striking changes are in the lobule. There is zonal centrilobular hepatocellular dropout, lymphoplasmacytic inflammation, congestion and hemorrhage. Focal central venulitis is also appreciated. Mild perivenular fibrosis is seen. However, there is also marked Kupffer cell hypertrophy, and reactive changes of hepatocytes including an increased nuclear:cytoplasmic ratio, spotty acidophilic necrosis of hepatocytes, and macronucleoli.
Compared to the previous biopsy there has been a marked increase in the centrilobular dropout and inflammation along with the congestion and hemorrhage.
Overall, the histopathological changes suggest that more than one process is contributing to the pathologic changes. First, the zonal centrilobular dropout with central plasmacytic inflammation and focal lymphocytic duct damage suggests a component of acute cellular rejection with central venulitis. However, it is difficult to explain the panlobular disarray, marked hepatocyte reactive changes, and Kupffer cell hypertrophy on the basis of rejection alone. These changes can be seen with hepatitis B viral infection of the liver, sepsis and reactive/regenerative change from vascular compromise, which last of which appears to have been excluded by imaging studies. Immunohistochemical stains to exclude HBV infection are suggested.
Lastly, the cause of the portal and periportal hemorrhage is uncertain. I have seen this change in intra-operative needle biopsies after vigorous manipulation of the liver for operative access, which presumably causes torsion between the portal tracts and the surrounding, less rigid, parenchyma. Other causes of portal and periportal hemorrhage include DIC and humoral rejection. However, none of these possibilities appear to be viable options based on the clinical profile and other histopathological findings.