Contributed by
Anthony Demetris, M.D.
Contributed by
Anthony Demetris, M.D.
PATIENT HISTORY: Per referral letter, the patient is a middle aged Saudi
male with end stage liver disease due to Hepatitis B who was transplanted. He has had good liver functions until quite recently. He developed a
persistent fever which has defied every work up. He has been cultured from every
site, scanned from head to toe, surgically explored, and biopsied in multiple
locations. An excisional biopsy of a supraclavicular lymph node turned out to be
a localized area of necrosis within the subcutaneous tissue. There is no real
granuloma formation or evidence of a pre-existing lymph node. All cultures have
been negative. No evidence of PTLD. He has been imperically treated with
numerous antibiotics, anti-fungal agents, and anti-tuberculous agents--all
without result. Currently, his serum chemistries are TB 15.9; AP 255; GGT 345;
AST 340; ALT 276, ALB 2.9; PT 13.8. His immunosuppression has been discontinued.
Review of outside material for followup.
Final Diagnosis (Case 23)
ALLOGRAFT LIVER, NEEDLE BIOPSY -
- TREATED ACUTE (CELLULAR) REJECTION, CURRENTLY, NO SIGNIFICANT ACTIVITY.
- LESS INFLAMMATION AND NECROSIS IN COMPARISON TO MOST RECENT PREVIOUS
BIOPSY (Case 22).
- BILE DUCT LOSS IN TWO OF FOUR (2/4) SMALL PORTAL TRIADS AND BILIARY
EPITHELIAL ATROPHY, SUGGESTIVE, BUT NOT DIAGNOSTIC OF THE EARLIEST PHASES OF
CHRONIC REJECTION (see microscopic description).
Previous Biopsies on this Patient:
Case 22
TPIS Related Resources:
Liver
Allograft Rejection Grading
Liver
Transplant Topics
Gross Description - Case 23
The specimen consists of two (2) consult
slides. No surgical pathology report is received with the specimen.
Microscopic Description - Case 23
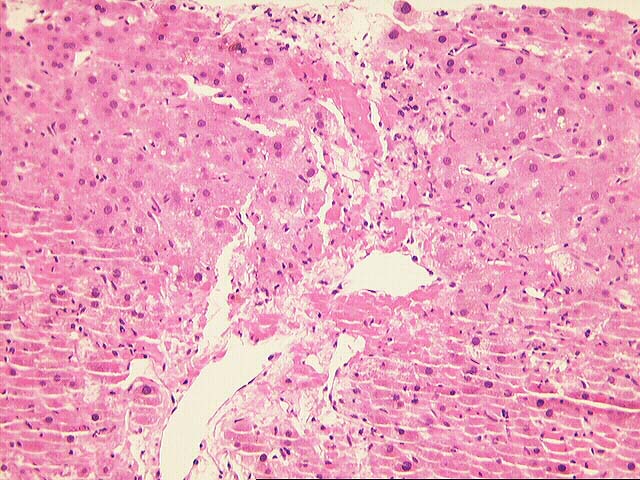
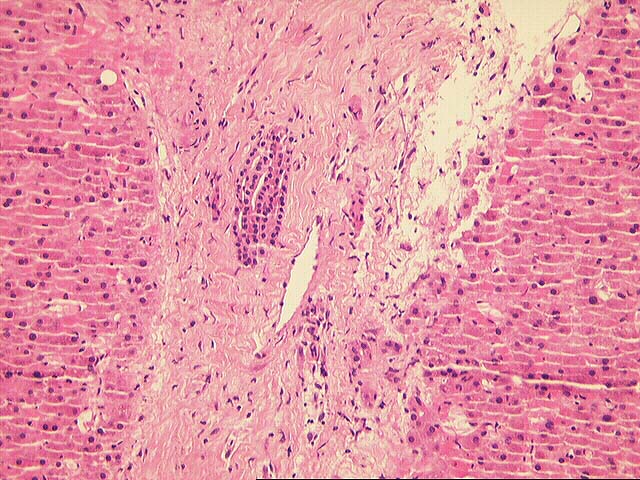
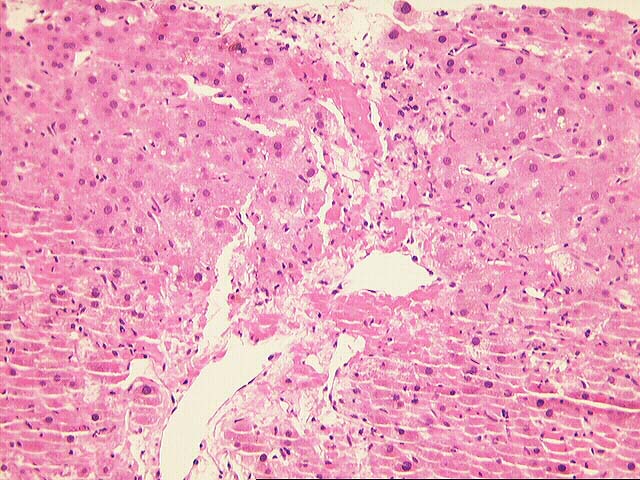
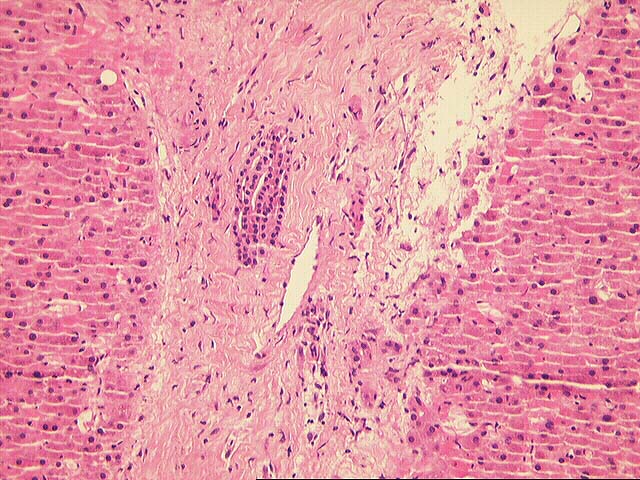
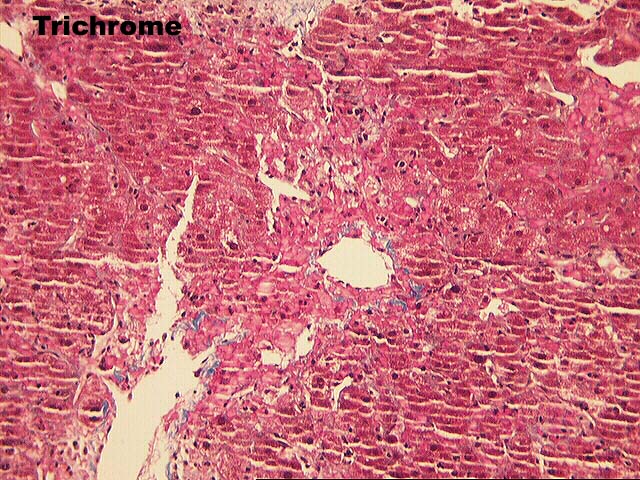
The normal lobular architecture is intact, but the biopsy is small and
fragmented. Four small and one large portal tract are identified. Approximately
three of the portal triads are either devoid of bile ducts or contain very small
atrophic biliary epithelial cells. There is no significant portal inflammatory
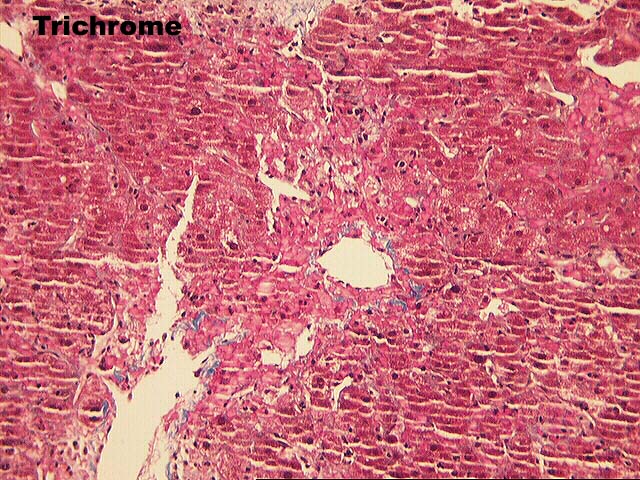
cell infiltrate, but the portal tract connective tissue appears slightly
collagenized.
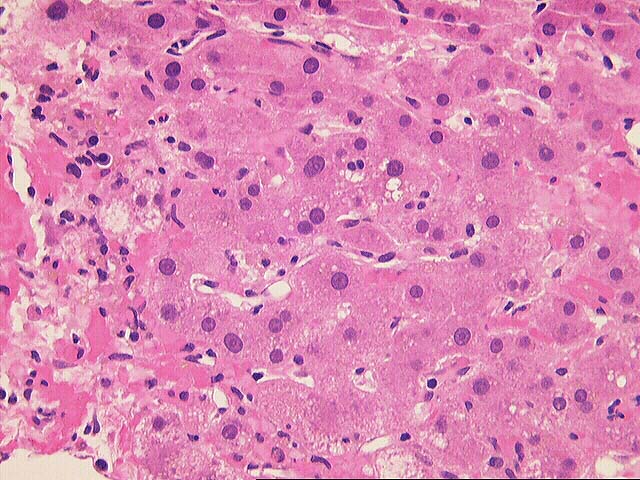
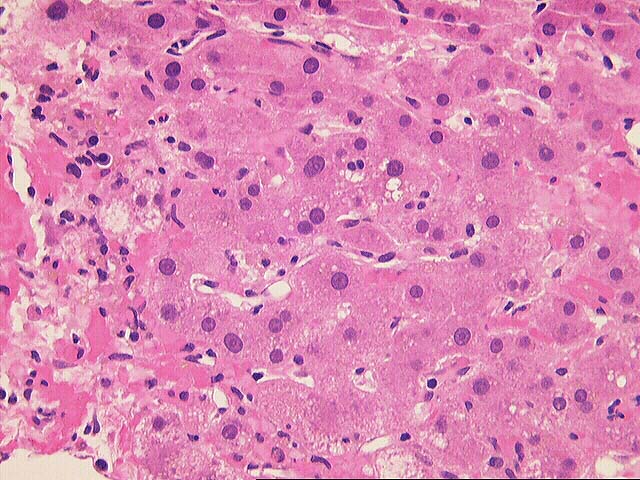
Throughout the lobules, there is Kupffer cell hypertrophy, thickening of the
plates, regenerative change, mild perivenular sclerosis and perivenular
hepatocellular swelling. No definite viral inclusions or ground glass cells are
seen.
Compared to the most recent previous biopsy (OSSL# D808-97), there has been a
decrease in the portal and perivenular inflammation and there is less
hepatocellular necrosis and dropout.
Overall, the histopathological changes are most consistent with a treated
acute rejection, which has improved since the previous sampling. Even though the
number of portal triads sampled is small, the loss of bile ducts in two and
atrophic changes into others are suggestive, but not diagnostic of the earliest
features of chronic rejection. If duct damage and loss is a widespread process
it should be clinically manifest by disproportionate elevations of the gamma
glutamyltranspeptidase and alkaline phosphatase. Rebiopsy to examine more portal
triads would help to substantiate the presence of ductopenia.
Please mail comments, corrections or suggestions to the TPIS administration at the
UPMC.