ACUTE INTERSTITIAL NEPHRITIS
Acute interstitial nephritis (AIN) refers to the presence of edema, inflammatory infiltration and tubular injury in the renal parenchyma. Acute rejection may be regarded as an immunologically mediated AIN. AIN can also be a manifestation of glomerulonephritis and allergic drug reactions. In this section, we will briefly consider biopsy findings in infectious AIN.
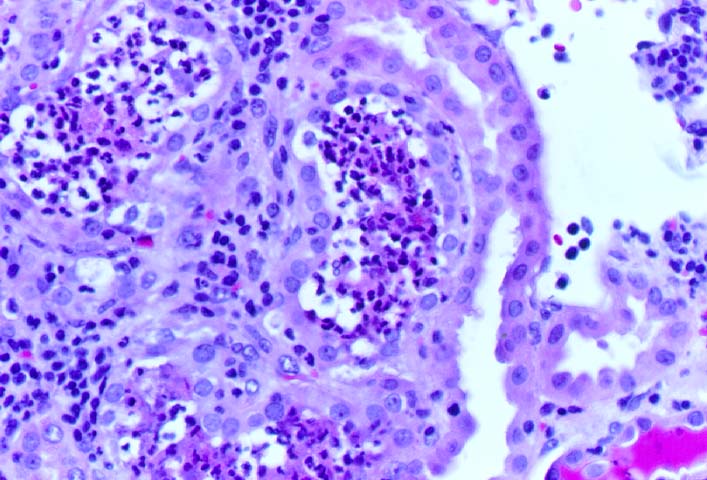
Bacterial AIN is recognized by dilated tubules containing clusters of neutrophils in the lumen. The interstitium may also show polymorphonuclear infiltrates and micro-abscess formation. The gram stain may be used to demonstrate cocciform or bacillary organisms in the infected kidney, but specific identification of the organisms involved requires urinary cultures.
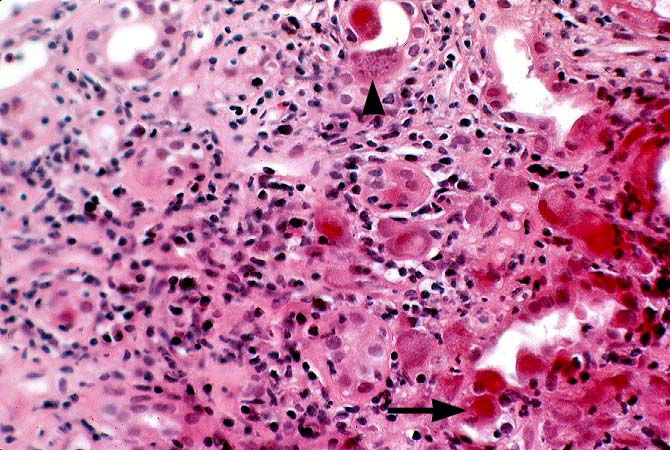
Cytomegalovirus(CMV) associated AIN is infrequent, even though CMV can be commonly cultured from the urine of renal transplant recipients. Specific biopsy diagnosis depends on the demonstration CMV inclusions in the tubular epithelium, vascular endothelium or inflammatory cells. In doubtful cases immunoperoxidase staining for immediate-early and early antigens is helpful in demonstrating CMV infection.
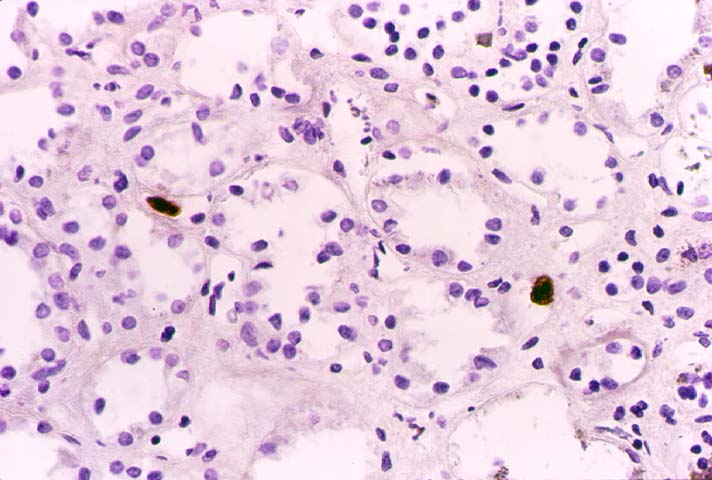
BK virus is another occasional cause of AIN. Histopathological diagnosis is based on the presence of viral inclusions primarily within the renal tubular epithelium. Definite identification may be done by immunohistochemistry, in-situ hybridization or electron microscopy. A more detailed discussion of this topic is presented separately.
Fungal infections may occasionally involve the renal allograft. The commonest example,Candida, is recognized by the presence of delicate pseudo-hyphae accompanied by budding yeast forms. The next most common organism is Aspergillus, which is recognized by septate hyphae branching in a dichotomous pattern. Rarely Cryptococcus, Histoplasma, and other fungi may be seen in allografts.
References
|
|
|