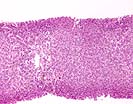
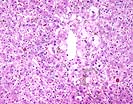
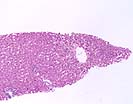
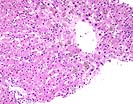
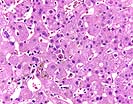
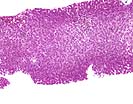
The second biopsy shows continued, but markedly improved, changes of preservation/ischemic injury with some residual Zone 3 hepatocellular swelling. A new finding in this biopsy is that of a mild lobular inflammation with mild to moderate numbers of necrotic hepatocytes. There is a mild ductular reaction within the portal tracts. No evidence for acute cellular rejection is seen.
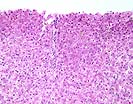
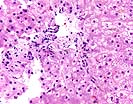
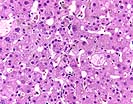
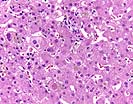
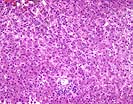
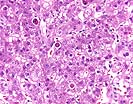
The third biopsy shows continued lobular inflammation and spotty necrosis, but in addition, shows mild cholestatic changes. There is also mild sinusoidal dilatation and congestion. The Kupffer' s cells and macrophages within the lobules and portal tracts continue to show moderately abundant green-brown pigment, which likely represents a mixture of iron and ceroid pigment.
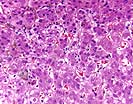
This series of biopsies shows mild to moderate preservation injury within the first biopsy, which shows significant improvement by the second and third biopsy. The abundant pigment in the Kupffer' s cells and macrophages likely represents a mixture of both a ceroid pigment and iron. By verbal report, an Iron stain showed abundant positivity. This ceroid deposition likely reflects "clean-up" activity from the mild to moderate preservation injury. In our experience, causes of increased iron deposits in Kupffer' s cells include hemolysis in ABO non-identical allografts, or hemolysis from other causes, aggressive exogenous iron therapy for anemia, transfusion and other sources of exogenous iron. Clinical correlation is recommended.
Overall, the histopathologic changes suggest that more than one insult is contributing to the liver allograft injury. The first process is that of ischemia/preservation injury, which is most prominent in the first sample and appears to be resolving. The most significant insult in the current sample appears to be attributable to recurrent hepatitis C viral hepatitis, as evidence by the marked acidophilic necrosis of hepatocytes, which is commonly the first histopathologic manifestation. The last biopsy also shows some cholestasis, which can be related to the hepatitis, or an additional insult, such as an adverse drug reaction. The former interpretation is favored. Lastly, the presence of cholestasis, minimal inflammation and mild ductular reaction in a patient with recurrent hepatitis C raises the possibility of a developing cholestatic hepatitis variant. Since over immunosuppression can favor the development of cholestatic hepatitis, continued clinical follow-up with careful monitoring of Hepatitis C viral load, immune suppression and rejection are suggested.
Any follow-up on this interesting and challenging would be appreciated.

University of Pittsburgh. All rights reserved. Unauthorized redistribution prohibited.