Contributed by Parmjeet Randhawa, M.D.
Contributed by Parmjeet Randhawa, M.D.
PATIENT HISTORY:
The patient is a middle aged married female. She does not smoke, nor indulge in alcohol. Takes no medications. About six months ago she developed silent jaundice. A sonogram showed cholelithiasis with a normal biliary tree. She underwent an open cholecystectomy. Following this procedure, her jaundice became more pronounced. Further evaluation included an ERCP that showed a normal biliary duct system. Serologic markers for hepatitis B and C, ANA, and ASMA were negative. An AMA gave a weakly positive response (1.2). Her liver function tests have remained consistent with cholestasis. Alb 3.1, SGOT/SGPT 172/202, GGT 942, albumin 3.1.
Final Diagnosis (Case 100)
PART 1:LIVER, NEEDLE BIOPSY -
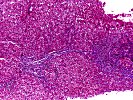
- GRANULOMATOUS PORTAL INFLAMMATION, WITH CHOLANGIOLAR PROLIFERATION, PERIPORTAL CHOLESTASIS, AND EARLY PORTAL TO PORTAL BRIDGING FIBROSIS.
- LOBULAR INFLAMMATION AND REGENERATIVE CHANGE, WITH FOCAL DUCT LOSS (3/17 DUCTS).
Microscopic Description - Case 100
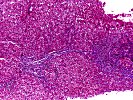
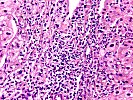
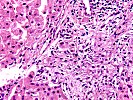
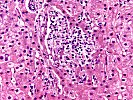
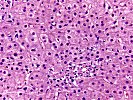
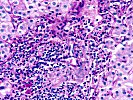
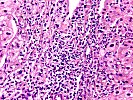
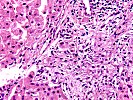
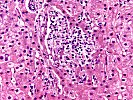
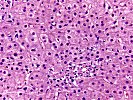
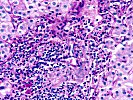
The needle biopsy contains a total of 17 portal triads, 3 of which appear to lack ducts. There is an active mononuclear inflammatory infiltrate, which focally causes duct injury, but no classic duct lesions are seen. A few plasma cells are noted. Two portal triads contain small collections of epithelioid cells. There is periportal cholestasis, cholangiolar proliferation, and sinusoidal form cell deposition. The lobule shows low grade inflammation and regenerative changes. There is no evidence for viral inclusions, Mallory' s hyaline, or significant fatty change. The central veins are essentially unremarkable. The trichrome stain shows frequent areas of early portal to portal bridging fibrosis. The PASD, orcein and iron stains are non-contributory. The copper stain is focally positive in periportal hepatocytes. The acid fast bacilli and fungal stains are negative.
In a middle aged woman with jaundice, these histopathologic changes warrant careful exclusion of primary biliary cirrhosis. Given the history of an equivocal AMA reaction, repeat testing including testing specifically for the mitochondrial antigen M2 is suggested.
Infectious causes of granulomatous inflammation are felt to be unlikely, but correlation with clinical and microbiologic information is needed. Grocott and acid fast bacilli stains performed in this laboratory were negative. Sarcoidosis should also be considered.
Final considerations in the differential diagnosis include AMA negative primary biliary cirrhosis, and injury secondary to drugs such as chlorpromazine, nitrofurantoin, tolbutamide, and non-steroidal anti-inflammatory agents.
Previous Biopsies on this Patient:
None
TPIS Related Resources:
None
Gross Description - Case 100
Received for consultation is one (1) consult block.
Photomicrographs - Case 100
Please mail comments, corrections or suggestions to the
TPIS administration at the UPMC.