It was the impression of the hepatologist at a second institution that the patient' s biopsy established cirrhosis and that she should be considered a candidate for liver transplantation.
There is a question of whether her recent liver functions reflect established cirrhosis or rather reflect an injured liver further compromised by cytomegalovirus, a process which may not necessitate a need for imminent transplantation.
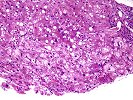
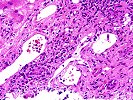
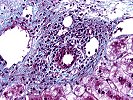
The portal tracts contain a mild to moderate inflammatory infiltrate composed of lymphocytes, plasma cells and occasional eosinophils. There is a ductular reaction present and occasional bile ducts show lymphocytic cholangitis. However, no classic florid duct lesions are seen.
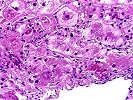
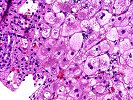
The lobules show cholestatic changes with occasional canalicular bile plugs, pseudorosette formation, foci of hepatocyte necrosis with aggregates of foamy histiocytes, and cholate stasis in the periportal hepatocytes. Mallory' s hyaline is prominent and is seen throughout some lobules including in zone 3. The central veins are generally unremarkable. A mild to moderate mixed micro macrovesicular steatosis is seen along with rare necrotic hepatocytes and a mild mixed lymphocytic and neutrophilic infiltrate within the sinusoids.
The Trichrome stain highlights the focal portal-to-portal bridging fibrosis. No significant pericellular fibrosis or central venular sclerosis is appreciated. A PASD stain is negative for intracytoplasmic globules. A PAS stain shows abundant glycogen. An Iron stain shows occasional positivity in Kupffer cells. A Reticulin stain highlights the reticulin framework and a vague nodularity. A CMV immunostain shows rare positive cells.
The chronic hepatitis is consistent with an autoimmune etiology, as suggested by the clinical history, but viral and drug causes should be excluded. Because of the lymphocytic cholangitis AMA are suggested. Superimposed on the background of chronic hepatitis, there are one or two cells that stain positively for CMV antigens, indicative of a superimposed CMV hepatitis. This is consistent with the history of immunosuppressive therapy.
There is also an active steatohepatitis as evidenced by Mallory' s hyaline and neutrophils within the lobules. Steatohepatitis is a non-specific pattern of liver injury that can be seen in association with obesity, diabetes, alcohol abuse, hyperlipidemia, drug toxicity, intestinal bypass surgery and other less common insults.
This very complicated biopsy shows features of several processes. First there is a background of chronic hepatitis with moderate architectural distortion, but short of end-stage cirrhosis. However, superimposed on this chronically injured liver are several acute processes, namely, steatohepatitis, CMV hepatitis and marked cholestasis with foam cell clusters. Based on the histopathological findings alone, I would suggest that both the chronic liver injury and acute insults are contributing to liver dysfunction. Regardless, histopathological evidence of either a lack of cirrhosis, or the presence of cirrhosis, should be clinically confirmed by searching for portal hypertension and other stigmata of chronic liver disease. The decision for liver transplantation should not be based on biopsy findings alone, or predominantly, since they are subject to sampling errors, especially in autoimmune hepatitis.
Lastly, the easily detectable Mallory' s bodies and foam cell clusters can be seen with prolonged cholestasis, either due to biliary tract disease, such as autoimmune cholangitis, choledocholithiasis, or functional cholestasis. Similar findings can also be seen in Wilson' s disease, but the patient' s age make this diagnosis unlikely. Regardless, the cholestasis appears to be out of proportion to the architectural abnormalities. Thus, liver function might appear to be worse than it otherwise might be, based on the architectural abnormalities alone. Thus, other possible factors contributing to the cholestasis, such as a biliary tract disease, sepsis or a drug reaction should be excluded.
Previous Biopsies on this Patient:
None
TPIS Related Resources:
None