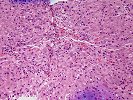
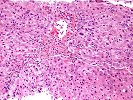
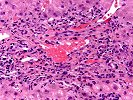
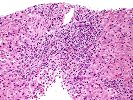
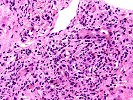
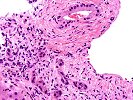
Sections of liver show architectural distortion by a prominent ductular reaction with accompanying portal fibrosis and a perivenular necro-inflammatory lesion. This results in focal portal-to-portal bridging. On closer examination, the portal tracts also contain a mixed inflammatory infiltrate composed of lymphocytes, neutrophils, plasma cells, and eosinophils. Many of the proliferated and some of the small native bile ductular showed marked atypia/atrophy/dysplasia, with cytoplasmic eosinophilia, uneven nuclear spacing and frank biliary epithelial cell necrosis with sloughing of the epithelial cells into the lumen of the ducts. This is associated with mononuclear and neutrophilic cholangitis. Scattered pigment laden macrophages are also present within the portal regions. Ductular-type interface activity is seen. The lobules show mild disarray with mild Kupffer cell prominence. There is a mild predominantly lymphocytic infiltrate within the sinusoids. Occasional necrotic hepatocytes are seen. Hepatocytes at the edge of the lobules show changes of cholatestasis with occasional foci of Mallory' s hyaline. There is also perivenular inflammation, congestion, hemorrhage, hepatocellular dropout and early fibrosis. Pigment laden macrophages are also present in these regions. A Trichrome stain highlights the fibrosis. An iron stain shows deposition within macrophages in the regions of the central veins as well as deposition within Kupffer cells throughout the lobules. A PAS/D stain is negative for intracytoplasmic globules. An Orcein stain is negative for viral inclusions and copper-associated protein.
Overall, the changes are most suggestive of an active graft versus host disease. This contention is based on the portal and perivenular inflammation, marked bile ductular atypia and the perivenular necro-inflammatory lesions. A ductular reaction can also be seen with GVHD, but we cannot exclude the possibility of an underlying biliary stricture, such as might be seen with primary sclerosing cholangitis(PSC), as suggested by the clinical history. However, PSC does not typically cause the perivenular necro-inflammatory lesions, or the marked biliary epithelial atypia seen in this specimen.
Because of the perivenular lesions, we also considered veno-occlusive disease(VOD), but felt it was less likely to be a contributing factor, based on the predominance of perivenular inflammation and dropout, in contrast to the predominance of congestion and hemorrhage typical of VOD; the lack of a clinical history of VOD and the time after transplantation(VOD usually occurs within the first month).
Lastly, any temporal association of the introduction of new drugs with the liver injury tests elevations is suggested, as an adverse drug reaction can cause similar changes. However, GVHD is the primary concern in a biopsy with marked ductular atypia and perivenular inflammation from an allogeneic bone marrow transplant recipient. I look forward to any follow-up in this case.
Previous Biopsies on this Patient:
None
TPIS Related Resources:
None