Comment:
The features in the biopsy point strongly to a chronic
biliary disorder that has evolved with bridging fibrosis and early cirrhosis. No
diagnostic bile duct lesions are present, but given the duct atrophy and only
modest inflammatory component, the most likely possibility is primary sclerosing
cholangitis or another form of low-grade biliary obstruction such as a duct
stricture. Drug-induced injury cannot be excluded, and primary biliary cirrhosis
and autoimmune cholangitis are less likely possibilities. Cholangiography should
be helpful in clarifying the nature and site of the obstruction; if the large
ducts are found to be uninvolved, a diagnosis of so-called small duct primary
sclerosing cholangitis should be considered. Previous Biopsies on this
Patient:
None
TPIS Related Resources:
Liver
Transplant Topics
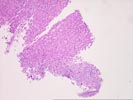
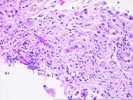
The liver biopsy is fragmented with zones of fibrosis focally present along their periphery. The parenchyma shows evidence of hepatic plate thickening and architectural irregularities. Although not definitive, this combination of changes suggests an evolving cirrhosis. The fibrous zones show focal ductular proliferation with duct atrophy, characterized by shrunken, disproportionately small ducts with nuclear hyperchromasia and irregularity, together with probable duct loss. The peripheries of the fibrous septa show loose, edematous connective tissue with intermingling of a sparse inflammatory infiltrate into the adjacent parenchyma, features indicative of a chronic cholestatic condition. Although no florid duct lesions or periductal obliterative fibrosis are seen, these changes along with the bile duct alterations point to a chronic biliary process. Because of the relative sparseness of inflammation within the fibrous septa, a diagnosis of primary sclerosing cholangitis is favored. However, similar appearances could be produced by other forms of low-grade biliary obstruction, by drug-induced duct injury, or less likely, by primary biliary cirrhosis or autoimmune cholangitis.