Comment:
The cause of the well-developed cirrhosis is not clearly
delineated. The location, size, and number of the PAS-positive
globules strongly suggests that the patient has at least one Z
allele for alpha-1-antitrypsin. However, we note from the
surgical pathology report that the serum AAT level was within
normal limits. To resolve this problem, phenotyping and
immunostains for alpha-1-antitrypsin may be necessary. In
addition, despite the reported presence of high titer microsomal
antibodies, the histologic features are not those typically noted
in (untreated) autoimmune hepatitis, although this possibility
cannot be completely excluded. Finally, several well-defined
epithelioid granulomas are seen in the PAS/D stain. Their
significance is not clear, but stains for microorganisms and
clinical workup for sarcoidosis may be useful. There is no
evidence for primary biliary cirrhosis or drug-induced injury.
Previous Biopsies on this Patient:
None
TPIS Related Resources:
Liver Transplant Topics
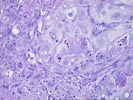
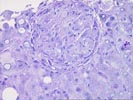
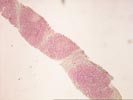
The liver biopsy shows hepatic architecture interrupted by a well-defined macronodular cirrhosis. This is characterized by portions of architecturally abnormal parenchymal nodules, partially bounded by irregular and dense fibrous septa. There is only minimal inflammatory activity with scattered mononuclear cells within the fibrous zones. Proliferated ductules are identified, and interlobular bile ducts are intact and without duct loss. The nodules are distinctive for the presence of numerous eosinophilic cytoplasmic globules, particularly in periseptal hepatocytes. These globules range greatly in size and number and are strongly PAS/D positive. This finding suggests the presence of at least one Z allele for alpha-1-antitrypsin deficiency and should be further worked up for the appropriate serum phenotyping. Otherwise, the nodules contain mild patchy macrovesicular steatosis and very minimal inflammation. At one end of the PAS/D stained section, two well-formed epithelioid granulomas are identified. These demonstrate a mild peripheral rim of collagen, but are not associated with active bile duct injury, caseation or necrosis, compartmentalizing fibrosis, or a cholestatic/hepatitic background. Their significance is not certain, but sarcoidosis and infections should be excluded.
Although the changes are indicative of an end-stage cirrhosis, histologic clues to the etiology are not identified. Some of the serum markers suggest the possibility of autoimmune hepatitis, that is not strongly supported by the histology (although the pathologic changes are not diagnostic).