Previous Biopsies on this Patient:
None
TPIS Related Resources:
Liver
Transplant Topics
(1 HE)
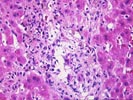
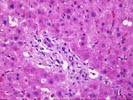
The normal lobular architecture is distorted by mild to moderate
portal fibrosis which is focally bridging. There is mild ductular proliferation
in some of the portal triads, but many of the ducts are atrophic appearing, show
eosinophilic transformation of the cytoplasm, uneven nuclear spacing and
pyknosis. There is also a mild predominantly mononuclear, but mixed inflammatory
cell infiltrate and mild portal edema. No obliterative arteriopathy is
recognized. Mild interface activity is seen.
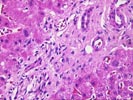
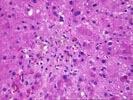
Throughout the lobules there is mild kupffer cell hypertrophy and mild to moderate spotty acidophilic necrosis of hepatocytes. However, no definite viral inclusions or ground glass cells are seen. There is however, perivenular hepatocellular dropout, congestion, hemorrhage, fibrosis and very mild perivenular inflammation.
The histopathological changes suggest that more than one insult is contributing to the liver injury. The portal fibrosis, which is focally bridging, and cholangiolar proliferation are consistent with a known history of recurrent primary disease in this patient. However, the widespread duct atrophy and pyknosis along with perivenular hepatocellular dropout and inflammation are somewhat unusual for recurrent primary biliary cirrhosis alone, and suggest a superimposed component of rejection, probably best classified as the early stages of chronic rejection. The spotty acidophilic lobular necrosis can be seen as part of the rejection syndrome, but viral infection, such as hepatitis B, hepatitis C and CMV infection should be excluded by serologic studies and immunohistochemical staining.