Previous Biopsies on this Patient:
None
TPIS Related Resources:
Liver
Transplant Topics
(1 HE)
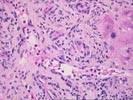
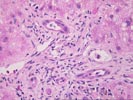
The normal lobular architecture is distorted by mild to moderate
portal expansion because of fibrosis, and a mild to moderate mixed inflammatory
cell infiltrate containing numerous eosinophils, focal ductular and cholangiolar
proliferation. No definite portal venulitis is seen, but duct infiltration and
damage are easily appreciated. In addition, there is portal edema and two or
three of approximately twelve to fourteen portal tracts are devoid of small bile
ducts. In addition, ductal atrophy and apoptosis are easily appreciated.
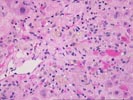
Throughout the lobule, there is mild Kupffer cell hypertrophy and an increased number of acidophilic bodies, but little evidence of lobular disarray. However, there is also zonal centrilobular hepatocellular necrosis and dropout with perivenular mononuclear inflammation. No definite viral inclusions or ground glass cells are seen.
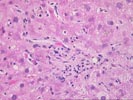
Overall, the histopathological changes suggest that more than one insult is contributing to allograft dysfunction. The portal tract edema and duct and cholangiolar proliferation, along with an increase in acute inflammatory cells is suggestive of biliary tract obstruction or stricturing, as previously suggested. In addition, the marked bile duct damage, increased portal eosinophilia, focal bile duct loss and zonal centrilobular hepatocellular dropout with inflammation and hemorrhage are suggestive of a superimposed acute rejection reaction, which is a new process since the previous biopsy.
Although, I cannot absolutely exclude the possibility of a co- existent hepatitis, rejection and biliary tract pathology appear to be the primary processes at this time.