PART 2:
ALLOGRAFT LIVER, NEEDLE BIOPSY -
- MILD ACUTE CELLULAR REJECTION.
- MILD ACUTE CELLULAR REJECTION, PARTIALLY TREATED.
- MINOR IMPROVEMENT COMPARED TO PREVIOUS BIOPSY.
PART 4:
ALLOGRAFT LIVER, NEEDLE BIOPSY -
- CHRONIC BILE DUCT INJURY WITH INTERLOBULAR BILE DUCTS MISSING FROM SIX FROM THIRTEEN (6/13) PORTAL TRACTS, CONSISTENT WITH EARLY EVOLVING CHRONIC REJECTION.
- HE STAIN NOT REVIEWED; ONLY CONNECTIVE TISSUE STAINS PROVIDED.
PART 5:
ALLOGRAFT LIVER, NEEDLE BIOPSY -
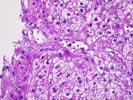
- CHRONIC BILE DUCT INJURY WITH INTERLOBULAR BILE DUCTS MISSING FROM SEVEN OF SEVENTEEN (7/17) PORTAL TRACTS, CONSISTENT WITH EARLY EVOLVING CHRONIC REJECTION.
- MILD DIFFUSE HEPATOCYTE SWELLING.
- FOCAL INTRALOBULAR DUCT DILATATION WITH ASSOCIATED MIXED
INFLAMMATORY REACTION.
Comment: The sequence of liver biopsies shows recurrent or persistent acute rejection progressing to early changes of chronic rejection. The chronic duct changes could also possibly result from hepatic artery stentosis, and if clinically indicated, this possibility should be addressed.
Previous Biopsies on this Patient:
NoneTPIS Related Resources:
Liver Transplant Topics
Gross Description (Case 74)
The specimen consists of ten (10) consult slides, Part 1 (3), Part 2 (2), Part 3 (2), Part 4 (2) and Part 5 (1) with an accompanying pathology report.
Microscopic Description (Case 74)

The explanted liver shows widespread hepatic necrosis with multilobular loss of liver cells, parenchymal collapse and profuse ductular proliferation. In less affected areas, a pattern of extensive bridging necrosis can be identified. Remaining liver cells are generally normal, although prominent cholestasis is noted. No particular etiology clues are identified, but the possibilities would include drug-induced injury, severe viral hepatitis, and, less likely, severe autoimmune hepatitis. Overall, however, no cause can be identified in some 30-40% of cases.
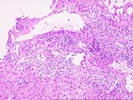
The first two biopsies (Parts 1 and 2) show similar changes with acute rejection characterized by regular portal inflammation by a mixed component of mononuclear cells and prominent eosinophils with occasional neutrophils. Mild duct damage is seen, but both portal and central subendothelial accumulations of cells is seen. These changes are characteristic of acute rejection. In addition, the second biopsy shows areas of portal tract edema together with ductular proliferation, features that can occur when previous acute rejection has been partially treated and may simulate biliary obstruction.
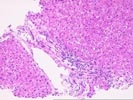
On the third biopsy (Part 3), we unfortunately received only a trichrome and a reticulin stain. Nonetheless, examination of the portal tracts demonstrates changes of chronic duct injury characterized by duct atrophy, nuclear enlargement and hyperchromasia, and dense cytoplasmic eosinophilia. In addition, bile ducts are absent from several portal tracts. These features suggest early ongoing chronic rejection. Similar findings are noted in the final biopsy (Part 5) in which chronic duct injury and duct loss are again appreciated. The hepatocytes show mild but diffuse cytoplasmic swelling. Although chronic rejection is the most likely possibility, hepatic artery stenosis can yield similar changes and, if relevant, should be excluded. No evidence to suggest recurrent hepatitis is noted.
Thank you for sending this case and I appreciate any follow up information you may receive.
Please mail comments, corrections or suggestions to the TPIS administration at the UPMC.
PART 3:
ALLOGRAFT LIVER, NEEDLE BIOPSY -