Previous Biopsies on this Patient:
None
TPIS Related Resources:
Liver
Transplant Topics
Part 1 (2 HE)
The normal lobular architecture is intact and greater than
eight to ten small portal tracts are identified, a few of which contain a mild
sprinkling of mononuclear cells. However, there is no significant duct damage or
duct loss. Mild cholangiolar reactivity is seen in some regions and mild mixed
steatosis is also present.
Overall, the changes in this biopsy are relatively mild and non specific.
Part 2 (2 HE)
The normal lobular architecture is basically intact, but
slightly distorted because of a vague nodularity, likely related to mild
intra-lobular regeneration. In addition, a few of the portal tracts contain a
mild mononuclear inflammatory cell infiltrate with very minimal focal duct
damage. No duct loss is appreciated. Within the lobule, there is thickening of
the plates and an increased number of mitotic figures, suggestive of low-grade
intralobular reactivity. Mild mixed steatosis is also present.
Overall, the changes in this biopsy are still relatively mild, but are suggestive of low-grade recurrent HCV.
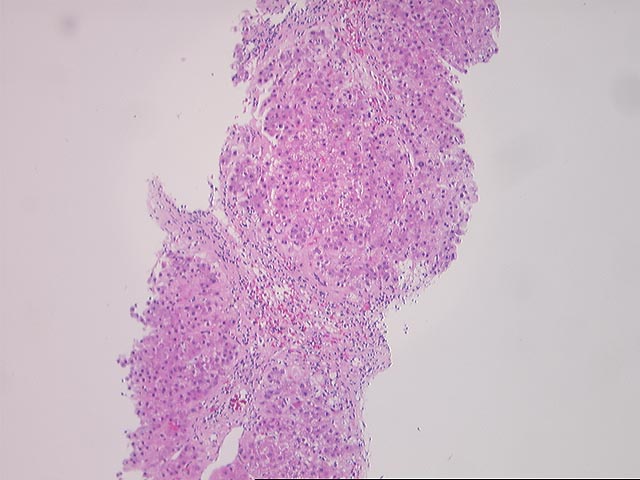
Part 3 (3 HE, 1 Trichrome)
There has been a dramatic change since the
previous biopsy. The normal lobular architecture is distorted by
portal-to-central, central-to-central and focal portal-to-portal bridging
necrosis/fibrosis. The remnant portal triads contain a mild to focally moderate
mononuclear inflammatory cell infiltrate. Although no portal venulitis is
appreciated, several ducts identified are distinctly atrophic or "dysplastic"
appearing, with eosinophilic transformation of the cytoplasm, uneven nuclear
spacing and ducts only partially lined by epithelial cells. In addition, a
minority of the portal tracts appear to be devoid of ducts.
Throughout the lobules, there is perivenular fibrosis and mild to moderate perivenular lymphoplasmacytic inflammation. There is also mild lobular disarray and occasional acidophilic bodies.
Overall, the changes present in this biopsy are indicative of an active rejection(acute and chronic) superimposed on a background of chronic hepatitis, viral type C by history, with the rejection being the more significant of the two processes. This contention is based on the perivenular distribution of the lobular inflammation; the ductulocentric portal inflammation and the marked bile duct damage and atrophy.
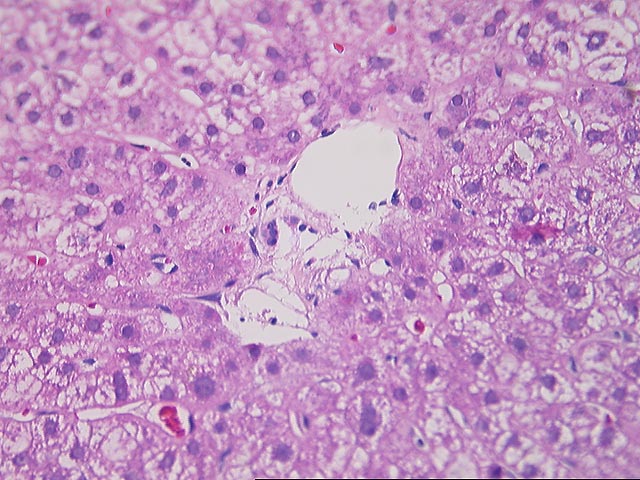
Part 4 (2 HE)
Compared to the previous biopsy, there is a marked decrease
in the perivenular and portal inflammation, but the architectural alterations
remain and there is still residual bile duct damage and atrophy/pyknosis with
three of eight (3/8) portal tracts devoid of ducts.
Overall, I would reconstruct this case as follows: The one-year follow-up biopsy was relatively unremarkable(Part 1) and the second biopsy(BS95-02406) shows low-grade changes indicative of recurrent Hepatitis C. The third biopsy(Part 2) shows marked deterioration because of an active (acute and early chronic) rejection superimposed on the background of chronic hepatitis, with rejection being responsible for most of the perivenular inflammation, duct damage and loss. It would be interesting to determine whether this patient was treated with interferon for the recurrent hepatitis. The relative contribution of hepatitis C and rejection to the architectural changes(bridging fibrosis) is difficult to determine with certainty, but in my opinion, both significantly contributed.
As might be expected, the fourth biopsy(Part 4) obtained after the switch to FK506 resulted in a significant decrease of the perivenular and portal mononuclear inflammatory cell infiltrate. Unfortunately, the architectural and ductal abnormalities persisted. Thus, at this point, the allograft is suffering from two serious insults: 1) duct damage and loss from rejection that is best classified as "early chronic rejection"; and 2) architectural alterations likely related to a combination of rejection and hepatitis. Although the rejection changes are still likely to be the most significant contributor to liver dysfunction(elevated gamma glutamyl transpeptidase, alkaline phosphatase and total bilirubin), there is potential for recovery since most of the active damage has subsided. Clinical correlation is required to determine if the architectural alterations have any affected portal pressures.