Comment:
On purely histologic grounds, the features seen would
suggest either viral hepatitis or autoimmune hepatitis as a cause of the
cirrhosis, but these have apparently been ruled out by appropriate serologic and
virologic testing. There is no evidence to support steatohepatitis, biliary
cirrhosis, alpha-1-antitrypsin deficiency or hemochromatosis as etiologies. This
case, therefore, appears to fall into that approximately 30% of cirrhotic livers
that remains cryptogenic.
Previous Biopsies on this Patient:
None
TPIS Related Resources:
Liver
Transplant Topics
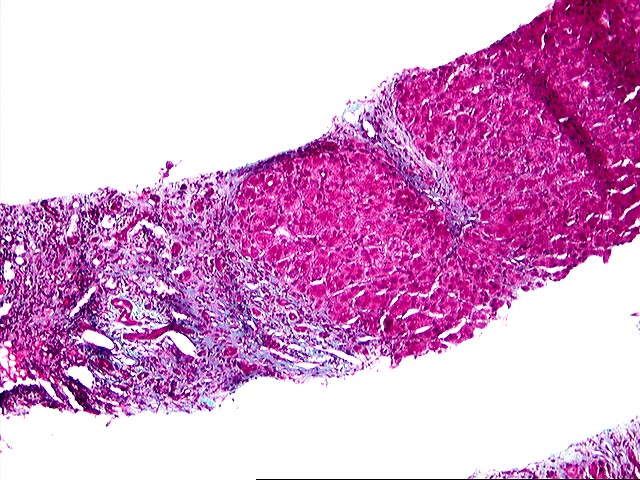
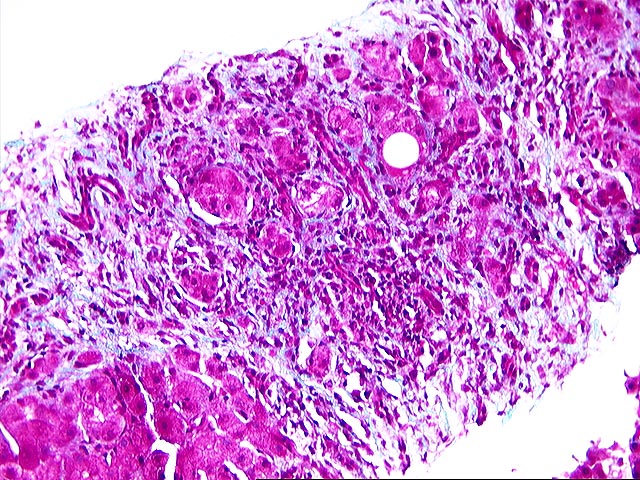
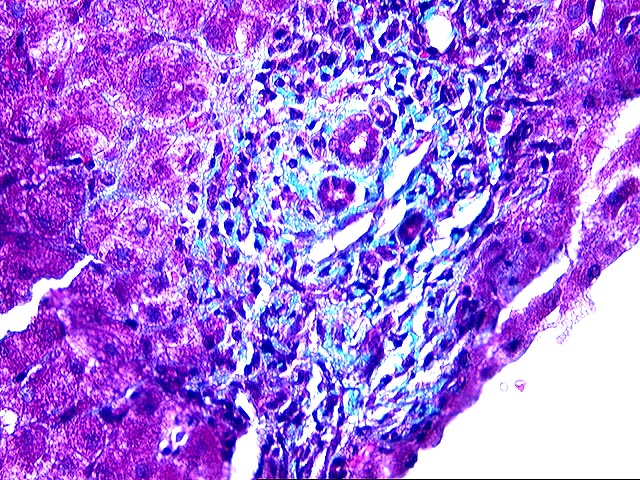
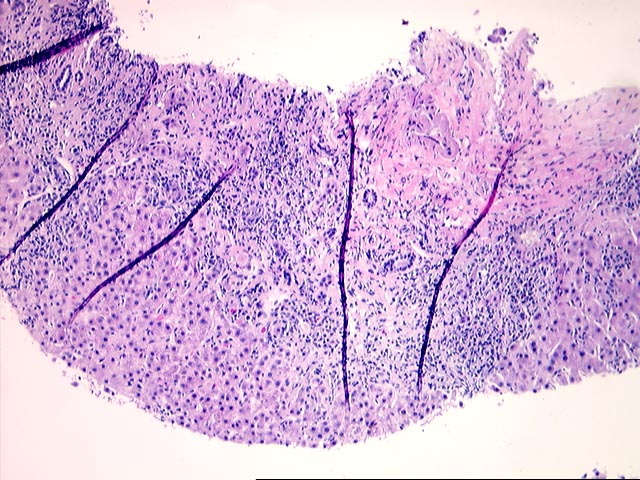
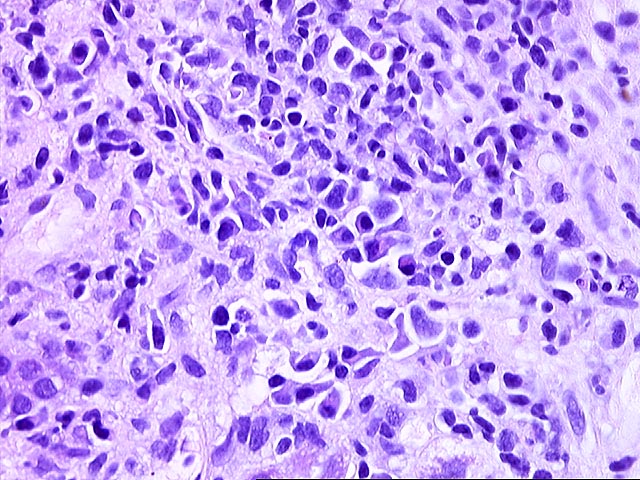
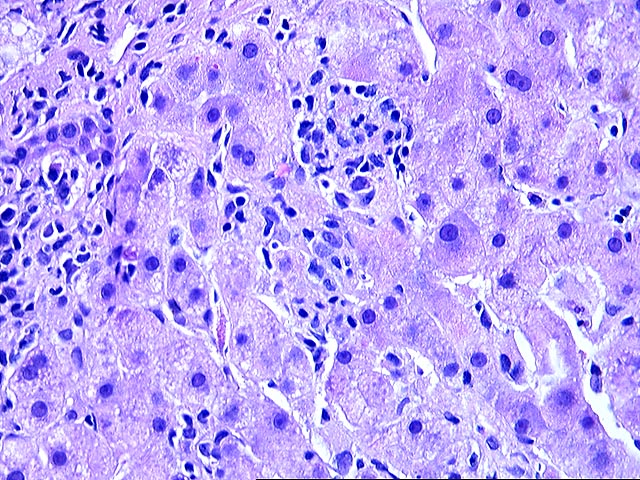
The liver biopsy shows zones of parenchymal collapse and fibrosis with early formation of parenchymal nodules, consistent with an evolving cirrhosis. The fibrous zones contain proliferated ductules and a patchy moderate mononuclear infiltrate, including lymphocytes and occasional plasma cells. There is mild to moderate piecemeal necrosis seen. Interlobular bile ducts appear intact. The lobules demonstrate moderate inflammatory infiltration with focal necroses and occasional acidophilic bodies. No ground glass hepatocytes, viral inclusions, cytoplasmic globules or pigment deposition are seen. There is no steatosis or evidence of steatohepatitis.
The appearances are those of an evolving cirrhosis, but no specific etiologic clues can be identified. The features do not suggest primary biliary cirrhosis, primary sclerosing cholangitis, hemochromatosis, Wilson's disease, or steatohepatitis.
Overall, the histologic appearances are most suggestive of a viral or autoimmune-induced cirrhosis, but these diagnoses will rest upon the clinical and laboratory features.