Previous Biopsies on this Patient:
None
TPIS Related Resources:
Liver Transplant Topics
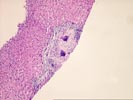
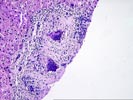
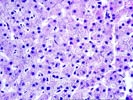
(2 HE) The normal lobular architecture is distorted by mild to moderate portal fibrosis which, shows focal early bridging, some of which is subcapsular. While the normal spatial relationship between portal tracts and central veins is maintained in some areas, the focal bridging results in distortion of this relationship in others. Thus, although there is significant architectural distortion, a well-developed cirrhosis is not seen.
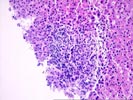
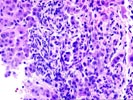
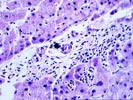
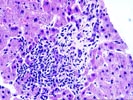
Mostly all of the triads contain a mild to moderate lymphoplasmacytic inflammatory cell infiltrate and one or two contain granulomas with multinucleated giant cells. Focal lymphocytic cholangitis, portal sclerosis and a paucity of small interlobular bile ducts with cholangiolar proliferation at the limiting plate are also seen.
The interface zone shows mild lymphocytic and ductular-type piecemeal necrosis.
The lobules show mild Kupffer cell hypertrophy and a slight increase in sinusoidal inflammatory cells with occasional apoptotic hepatocytes. No prominent pigment deposition, nor Mallory's hyaline, nor steatosis nor significant cholestasis are seen.
Assuming that the AMA is the M2 variant, I would agree that the histopathologic changes are indicative of primary biliary cirrhosis. Each of the other less likely possibilities including a drug reaction, deep fungal or mycobacterial infection and sarcoidosis are addressed below.
Three out of the four drugs which this patient is receiving are potentially hepatotoxic and their metabolism can be impaired in the face of chronic liver disease. In addition, other, non-M2 AMA variants can uncommonly be seen with adverse drug reactions(Larrey, D. Rev Med Interne 16 (10): 752-758, 1995). However, none of the drugs mentioned has commonly been associated with a PBC-like syndrome, which is more often seen with the phenothiazines.
Sarcoidosis can also mimic PBC in about 10-15% of cases, but other clinical and laboratory findings are usually present and periportal, as well as portal, granulomas are usually detected(Devaney K, Goodman ZD, Epstein MS, Zimmerman HJ, Ishak KG. Am J Surg Pathol 17 (12): 1272-1280, 1993). Deep fungal or mycobacterial infections are also less likely considerations. Clinical correlation and stains for micro-organisms are suggested to exclude both sarcoidosis and infectious possibilities.
In summary, PBC is the leading consideration and the diagnosis can be further substantiated by subtyping the AMA, and clinically excluding the other much less likely possibilities mentioned above.