Previous Biopsies on this Patient:
None
TPIS Related Resources:
Liver Transplant Topics
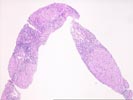
(3 HE, 1 Reticulin) The normal lobular architecture is replaced by a mildly active, mixed micro- and macronodular cirrhosis. The normal spacing between portal tracts and central veins is disrupted in most areas. In addition, one or two nodules surrounded on at least three sides by fibrosis are seen. There are also several large areas of parenchymal extinction. However, as always, a histopathological diagnosis of cirrhosis should be clinically confirmed by searching for portal hypertension and other stigmata of chronic liver disease.
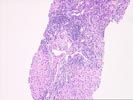
On closer examination, the portal tracts/fibrous septae show a mild to moderate, predominantly mononuclear inflammatory cell infiltrate which is focally arranged into nodular aggregates. However, bile ducts appear intact and no florid duct lesions are seen. There is mild ongoing interface activity.
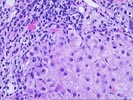
Throughout the lobules/nodules, there is thickening of the plates, Kupffer cell hypertrophy, occasional acidophilic bodies and a slight increase in pigment, which appears to be iron present in both reticuloendothelial cells and hepatocytes. No granulomas are identified. No definite ground glass cells are seen.
The clinical profile given, mentions a history of significant Tegretol exposure, as well as positivity for hepatitis B and C virus infections and possible ethanol intake. However, review of the actual data for the serologic testing reveals apparent immunity to the B virus, and no definite documentation of hepatitis C virus infection.
The histopathological changes alone, are most consistent with chronic hepatitis C virus infection, but this cannot be determined with certainty until persistent viral infection has been documented. There is no definite evidence of ethanol abuse, as suggested by the clinical history. The history of long Tegretol exposure is of interest, particularly when a known association between chronic Tegretol exposure and liver injury exists. However, the majority of Tegretol-associated liver injury show a granulomatous response, which was not present in the current sample. Therefore, while the possibility of drug- induced injury cannot be entirely excluded, it is considered a less likely possibility. Thus, our leading consideration at this time would be chronic hepatitis C virus infection, pending addition laboratory testing and clinical information.