Previous Biopsies on this Patient:
None
TPIS Related Resources:
Liver Transplant Topics
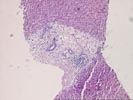
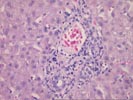
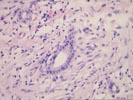
(3 H&E, 1 Trichrome, 1 PAS) The normal lobular architecture is mildly distorted because of mild portal expansion because of edema, minimal fibrosis and a mild inflammatory cell infiltrate, focally enriched with neutrophils. There is duct and cholangiolar proliferation and acute inflammatory cells can be seen in between the biliary epithelial cells and in the ductal lumen. Similar changes are present in a small septal duct at one end of the needle core. This portal tract in particular shows periductal edema and a neutrophilic and eosinophilic inflammatory response.
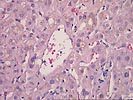
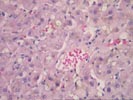
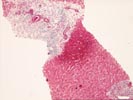
Throughout the lobules, there is marked centrilobular hepatocanalicular cholestasis and Kupffer cell hypertrophy. Occasional acidophilic bodies are seen, but these are not plentiful. No viral inclusions or ground glass cells are seen however, there is an increased mitotic rate within the lobules, which is suggestive of recent hepatocellular turnover. Prominent pigment deposits are present.
Overall, the combination of duct and cholangiolar proliferation with portal neutrophilia and marked centrilobular cholestasis are most consistent with biliary tract obstruction or stricturing. This should absolutely be excluded by cholangiography. Because of the marked cholestasis and minimally distorted architecture, we would favor an acute process such as choledocholithiasis and/or an acute cholangitis. Other more chronic causes of mechanical biliary tract compromise include biliary tract tumors, infections and sclerosing cholangitis, seem less likely in this case. Clinical correlation with follow-up should help to distinguish between these possibilities. Lastly, acute hepatitis A and other forms of cholestatic hepatitis can occasionally show a cholestatic histological profile and mimic biliary tract obstruction. I look forward to any follow-up in this case.