Comment:
No evidence of active steatohepatitis is seen.
Previous Biopsies on this Patient:
None
TPIS Related Resources:
Liver Transplant Topics
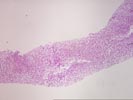
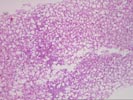
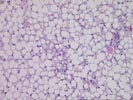
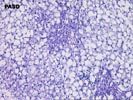
The liver biopsy shows intact hepatic architecture, but there is marked diffuse steatosis involving virtually the entire specimen. This is generally macrovesicular steatosis, although foci of microvesicular fat is focally seen. An occasional inflammatory cell is present in the lobule but no Mallory bodies or evidence of steatohepatitis seen. The portal tracts are mildly expanded with ductular proliferation, a loose scattering of primarily neutrophils and focally ductular cholestasis is seen.
The portal changes suggest a reactive process either to sepsis or some other systemic or intraabdominal process. In this case presumably the severe acute inflammatory bowel disease is responsible. The cause of the steatosis is not evident but causes such as obesity, diabetes mellitus, relative malnutrition and perhaps steroids could contribute. Although acute cholangitis is a possibility given the ductular proliferation and neutrophil infiltration, the lack of significant edema makes this unlikely. If this remains a clinical possibility appropriate imaging techniques may be required.