Comment:
The combination of histologic changes in this cirrhotic liver,
including the loss of bile ducts, points strongly to a biliary
etiology. Cholangiography or other means of bile duct imaging
should therefore be considered in order to exclude priamry
sclerosing cholangitis and other forms of biliary obstruction.
Other diagnostic possibilities include bile duct paucity
syndromes and alpha-antitrypsin deficiency (although this has
apparently been excluded biochemically).
Previous Biopsies on this Patient:
None
TPIS Related Resources:
Modified Knodell Scoring
Liver Transplant Topics
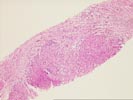
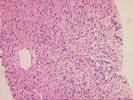
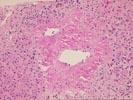
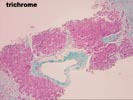
The liver biopsy show hepatic architecture deranged by a well- developed, predominantly micronodular, cirrhosis. There is a zone of subcapsular parenchymal collapse, but deeper in the specimen, the fibrosis is primarily portal-based. Most striking is the absence of many intralobular bile ducts, although ductular proliferation is seen. There is mild interface inflammatory activity together with the proliferated ductules and loose connective tissue proliferation at the nodular periphery. These changes are indicative of a chronic cholestatic condition. The lobules are largely unremarkable, although dense zones of fibrosis surrounds several of the terminal hepatic venules. The cause and significance of this change is unclear, although the possibility of an underlying vascular malformation should be kept in mind.
The combination of histologic features points to an ongoing biliary process with primary sclerosing cholangitis or a bile duct paucity syndrome among the most likely possibilities. Other less likely considerations include alpha-1-antitrypsin deficiency, autoimmune cholangitis, drug induced ductopenia and idiopathic cases.