Contributed by Michael A. Nalesnik, M.D.
Contributed by Michael A. Nalesnik, M.D.
PATIENT HISTORY:
Per referral report, the patient is a 54-year-old white female
with significant history of hypertension, prior biliary
cirrhosis. The patient presented to the office seeing me on the day
of admission complaining of two-day history of increasing
fatigue, legs giving out, lightheadedness and nausea, diaphoresis
when she would stand or be active. Also on questioning she did note
dark stools. The patient has a significant history of taking two
aspirin q night for approximately 10 years, also one glass of
wine every night and drinking one to two cups of coffee in the
morning. Approximately one to two weeks prior to this, the
patient noted myalgias and pharyngitis. She was started on antibiotics and also increased her aspirin intake secondary to the myalgias.
In my office, the patient was found to have an orthostatic tilt.
Conjunctive were pink. The patient had regular rhythm and tachy
when she sat up. Abdomen was fairly soft with occasional
tenderness in the lower quadrants. Rectal revealed significant
black stool. Hematocrit in the office was 23. The patient was
transferred by ambulance to the hospital as a direct admission for continued evaluation and care.
Final Diagnosis (Case 50)
PART 1: NATIVE LIVER, NEEDLE BIOPSY (5/2/97) -
- CHRONIC HEPATITIS WITH PORTAL FIBROSIS (see comment).
PART 2: NATIVE LIVER, NEEDLE BIOPSY (10/18/84) -
- LIVER WITH REDUCED NUMBERS OF BILE DUCTS, FOCAL DUCTULAR PROLIFERATION AND PERIPORTAL FIBROSIS, COMPATIBLE WITH THE CLINICAL HISTORY OF PRIMARY BILIARY CIRRHOSIS.
Comment:
The changes in the 1984 biopsy, namely, reduced numbers of bile
ducts and biliary-type piecemeal necrosis, are compatible with
the clinical history given that this patient has primary biliary
cirrhosis. Supportive laboratory evidence strengthen this
opinion.
The more recent biopsy shows apparent progression of changes in
the form of slightly more prominent portal fibrosis. I agree
that the findings fall short of cirrhosis at this time. In
addition, the findings in the most recent biopsy, taken alone,
are non specific. However, when combined with the earlier
biopsy, the findings can be considered as consistent with the
patient's underlying disease.
Previous Biopsies on this Patient:
None
TPIS Related Resources:
Modified Knodell Scoring
Liver Transplant Topics
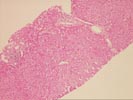
Gross Description - Case 50
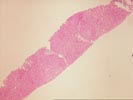
The specimen consists of two (2) consult slides,Part 1,
(1) and (1),Part 2, both with their respective blocks (1 each), with
accompanying surgical pathology reports and patient history.
Microscopic Description - Case 50
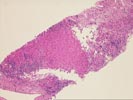
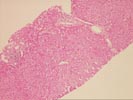
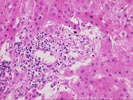
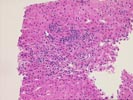
The slide,Part 1, shows bridging fibrosis with patchy
inflammation, primarily at the interface regions. Some ductular
proliferation is, again, noted and a questionable reduction in
bile ducts is appreciated. The uncertainty arises from the small
number of identifiable portal tracts seen. The hepatocytes are
unremarkable and occasionally contain mild macrovesicular fat
globules.
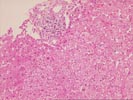
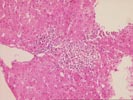
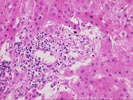
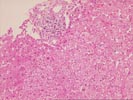
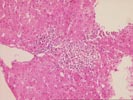
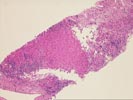
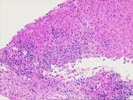
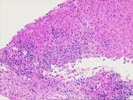
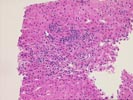
The slide,Part 2,consists of a needle core of hepatic
parenchyma with portal inflammation and expansion. The portal
tracts contain occasional bile ducts which are partially
disrupted by the predominantly mononuclear inflammatory
infiltrate. In addition, rare eosinophils are noted. In other
portal areas, bile ducts are not seen. Occasional foam cells are
noted at these sites. Enlargement of portal tracts raises the
possibility of early bridging in some sites. Focal ductular
proliferation is noted at the limiting plate regions.
Please mail comments, corrections or suggestions to the
TPIS administration at the UPMC.