Previous Biopsies on this Patient:
None
TPIS Related Resources:
Modified Knodell Scoring
Liver Transplant Topics

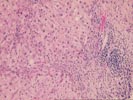
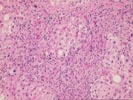
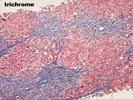
(1 H&E, 1 Trichrome, 1 Iron, 1 Reticulin) The normal lobular architecture is replaced by an active, predominantly micronodular cirrhosis. The normal spatial relationship between the portal tracts and central veins has been disrupted in most areas and the trichrome stain shows nodules surrounded on all four sides by fibrosis. As always, a histopathologic diagnosis of cirrhosis should be clinically confirmed by searching for portal hypertension and other stigmata of chronic liver disease.
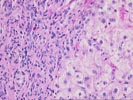
Remnants of the portal tracts within the fibrous septae show marked bile duct proliferation, accompanied by a largely acute inflammatory cell infiltrate. No florid or granulomatous duct destructive lesions are seen. No definite fibro-obliterative duct lesions are identified.
At the interface zone, there is marked cholangiolar proliferation and acute cholangiolitis. Periportal hepatocytes are swollen and show cholatestasis-type changes. No prominent pigment deposition or ground glass cells are seen. No significant dysplasia is appreciated. There is mild, predominantly macrovesicular steatosis. A rare periseptal hepatocyte contains Mallory's-like hyaline. There are no increased iron stores present.
Overall, the histopathological changes are indicative of chronic liver disease with advanced architectural distortion, that has a distinct "biliary" appearance. This contention is supported by the marked ductular proliferation, the portal and periportal neutrophilia, and the cholatestasis-type changes in the periportal regions and the marked elevation of the alkaline phosphatase and gamma glutamyltranspeptidase. Possibilities would include partial and/or intermittent biliary tract obstruction or stricturing, such as might be seen with primary sclerosing cholangitis, a biliary tract neoplasm or other mechanical problem, such as a biliary tract stone. Primary biliary cirrhosis is unlikely because of the intact small bile ducts, lack of non-suppurative cholangitis and the negative AMA.
However, this case is somewhat puzzling because an ERCP with contrast injection of the biliary tree is reportedly normal. If indeed biliary mass lesions and obstructive cholangiopathy have been confidently excluded, other possibilities for the histopathologic changes would include an autoimmune hepatitis. Anti-nuclear antibody, anti-neutrophil cytoplasmic antibodies(ANCA) and anti-liver membrane protein(LMP) antibody testing would provide other useful information. Lastly, if all of these diagnoses have been excluded, it is possible but not likely, that the precursor lesion was non-alcoholic steatohepatitis. I look forward to any follow-up in this case.