Previous Biopsies on this Patient:
None
TPIS Related Resources:
Knodell Scoring
Liver Transplant Topics
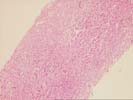
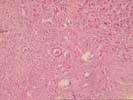
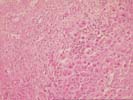
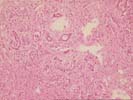
The liver biopsy shows a well-established cirrhosis with generally small parenchymal nodules bounded by dense zones of collapse and fibrosis. The fibrous septa contain minor, predominantly mononuclear infiltrate, together with dense zones of proliferated ductules; plasma cells are rare. In addition are several areas of paucicellular fibrosis, some of which are associated with apparent obliterated central veins, and rare interlobular bile ducts appear sclerotic. The parenchymal nodules show mild hepatocyte swelling with occasional focal necrosis, and minor piecemeal necrosis. Occasional nodules show slight swelling of the periseptal hepatocytes with interdigitating loose connective tissue. No steatosis, active steatohepatitis, ground glass hepatocytes, viral inclusions, cytoplasmic globules, or pigment deposition is seen.
Overall, the changes are those of an end-stage cirrhosis, and there are few clues to its etiology. On the basis of the micronodularity and foci of dense paucicellular fibosis, inactive alcoholic cirrhosis would be a likely diagnosis. The lack of substantial inflammation argues against autoimmune hepatitis, assuming that the patient has not been receiving immunosuppressive therapy. Finally, some of the features raise the possibility of an underlying biliary obstruction, and, if clinically indicated, biliary imaging might be useful in excluding this possibility.