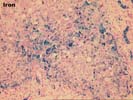
An attached iron index calculation from American Medical Laboratories(see attached report) is 3.1 umol/g/yr, with a normal of 1.0. Results > 1.9 are said to indicate homozygous hemochromatosis or transfusion-related iron overload.
Previous Biopsies on this Patient:
NONE
TPIS Related Resources:
Knodell Scoring
Liver Transplant Topics
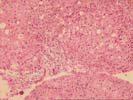
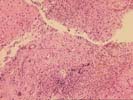
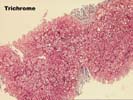
The biopsy is small and fragmented. Some of the fragments are rounded on the edges and surrounded by fibrous tissue, at least on three sides. In addition, the normal spatial relationship between portal tracts and central veins is destroyed in most areas, but maintained in one small region.
The portal triads and fibrous tracts contain a mild to focally moderate, predominantly mononuclear inflammatory cell infiltrate, which is focally arranged into nodular aggregates. Bile duct damage and loss are not seen. The infiltrate spills over into the edge of the lobules where moderate interface activity is seen.
Throughout the lobules/nodules, there is mild macrovesicular steatosis, Kupffer cell hypertrophy, thickening of the plates and occasional acidophilic bodies. One of the most striking changes is the presence of marked iron deposition, which is present both in Kupffer cells and hepatocytes. In addition, marked deposits are also seen in periportal cholangioles and biliary epithelium, which is unusual for a secondary overload.
Overall, the histopathological changes are most consistent with a bridging fibrosis/early cirrhosis, which should be clinically confirmed by searching for portal hypertension and other stigmata of chronic liver disease. The most significant underlying etiology at this time appears to the chronic Hepatitis C virus infection. This contention is based on the presence of advanced architectural abnormalities in conjunction with the chronic portal inflammation and inflammatory interface activity, which are unusual for hemochromatosis alone. However, the iron deposits are likely contributing to the injury.
The iron deposits, which are 3+ on histopathological staining, show a mixed distribution pattern. The most likely possibility is that this represents a primary genetic defect in iron metabolism(hemochromatosis) with redistribution of iron because of the overlapping viral hepatitis. The other possibility is that the iron overload is secondary. The former interpretation is favored because of the marked deposits in biliary epithelium, cholangioles and periportal hepatocytes; the high hepatic iron index(3.1); and no given history of anemia or exogenous iron overload. Genetic testing to search for the gene defect would be warranted.
This case has also been reviewed by Dr. Lee, who concurs with the interpretation.