Previous Biopsies on this Patient:
NONE
TPIS Related Resources:
Liver Allograft Biopsy Rejection
Criteria
Liver Transplant Topics
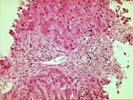
Both biopsies are similar in appearance and, therefore, will be described together with most of the description devoted towards the more recent sample (1/9/97).
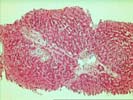
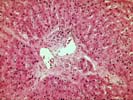
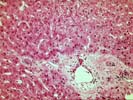
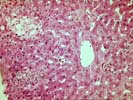
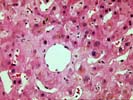
The normal lobular architecture is distorted by mild portal expansion because of mild fibrosis and focal cholangiolar reactivity. However, there is no significant portal inflammation. There is, however, widespread bile duct atrophy and pyknosis. In addition, there is a decrease in bile ducts; in total, there are 13 triads and at least five are devoid of bile ducts. The portal tract connective tissue is also somewhat collagenized and more dense than usual.
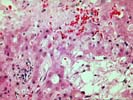
Throughout the lobule, there is minimal evidence of disarray. However, there is marked centrilobular hepatocanalicular cholestasis, focal areas of hepatocellular dropout, clusters of intrasinusoidal foam cells and occasional foci of extramedullary hematopoiesis. No definite viral inclusions or ground glass cells are seen.
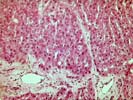
Overall, the histopathological changes are suggestive of ongoing bile duct injury and focal bile duct loss. This can be a manifestation of chronic rejection, severe hepatic artery narrowing and/or obstruction and biliary tract obstruction or stricturing. It is difficult to absolutely distinguish between these possibilities with certainty in a core needle biopsy because the pathophysiological mechanisms of duct injury in these different circumstances can be quite similar. Severe cholestasis as a result of chronic rejection can also occasionally cause the small areas of bile necrosis, which are more usually seen with biliary obstruction. In addition, arterial narrowing and/or obstruction either from technical problems or chronic rejection, can result in biliary tract obstruction or stricturing and atrophic changes in some of the small bile ducts. Thus, arterial and biliary problems can, and often are, overlapping.
In this case, I would favor a diagnosis of chronic rejection because of the widespread nature of the bile duct atrophy and pyknosis, the portal tract collagenization, the bile duct loss and the relative paucity of periductal edema. However, before instituting any specific therapy, investigation of the arterial and biliary tree is probably warranted. I look forward to any follow-up in this case.