Contributed
by Anthony J. Demetris, M.D.
Contributed
by Anthony J. Demetris, M.D.
PATIENT HISTORY: Per referral letter, the patient is a middle aged black
male who underwent liver transplantation for acute fulminant liver
failure due to Budd-Chiari syndrome. De novo post transplant hepatitis C was
diagnosed by HCV RNA in serum and liver tissues and a
consistent histopathological features. His aminotransferases and total bilirubin
were persistently elevated between 1-2 times normal until early November when
the total bilirubin and alkaline phosphatase were noted to be 5 times normal.
Itaconazole, started about 2-3 weeks earlier for dermatophytosis, was
discontinued due to presumed hepatotoxicity. His other medications were
cyclosporine A, prednisone, coumadin, and axid. Subsequently, the patient
developed a progressive rise in AST, ALT and total bilirubin to 700-900,
1200-2100 and 25-30 mg/dl. He has been on anticoagulant therapy and recent
ultrasound with Doppler flow studies indicate that all hepatic vessels are
patent. An ERCP was normal. A CT scan of the abdomen showed ascites, but no mass
or lymphadenopathy. All viral studies (HAV, HBV, CMV, EBV) have been negative.
Serum HCV RNA levels have not changed compared to earlier when his condition was
stable. A qualitative EBV PCR was positive but EBV DNA was undetectable by a
quantitative assay (done at the University of Pittsburgh). An EBER in situ
hybridization study was equivocal, but since B cells were uncommon in the liver
infiltrate post transplant lymphoproliferative disorder is unlikely. He has had
several liver biopsies which showed chronic hepatitis, more recently with
cirrhosis and features of acute hepatitis. Despite 2 weeks of interferon for
possible hepatitis C and empiric ganciclovir (?EBV), his condition has not
improved. The patient now has ascites, hepatic encephalopathy, hypoalbuminemia,
and renal failure. Review of outside material.
Final Diagnosis (Case 10)
ALLOGRAFT LIVER, NEEDLE BIOPSY Part 1-
- ACTIVE HEPATITIS, VIRAL TYPE C, FEATURES OF ACUTE WITH TRANSITION TO
CHRONICITY.
- FOCALLY BRIDGING FIBROSIS.
- SUPERIMPOSED ACUTE CELLULAR REJECTION, MILD, WITH DUCT DAMAGE(see
microscopic description).
ALLOGRAFT LIVER, NEEDLE BIOPSY Part 2-
- ACTIVE HEPATITIS, VIRAL TYPE C, FEATURES OF ACUTE WITH TRANSITION TO
CHRONICITY.
- FOCALLY BRIDGING FIBROSIS.
- LESS PORTAL INFLAMMATION AND LYMPHOCYTIC DUCT DAMAGE IN COMPARISON TO
PREVIOUS BIOPSY, CONSISTENT WITH INCREASED IMMUNOSUPPRESSIVE THERAPY.
- RESDIUAL DEGENERATIVE CHANGES IN SMALL BILE DUCTS, SUGGESTIVE OF THE
EARLIEST PHASES OF CHRONIC REJECTION(see microscopic description).
Previous Biopsies on this Patient:
NONE
TPIS Related Resources:
Liver
Allograft Biopsy Rejection Criteria
Liver
Transplant Topics
Gross Description - Case 10
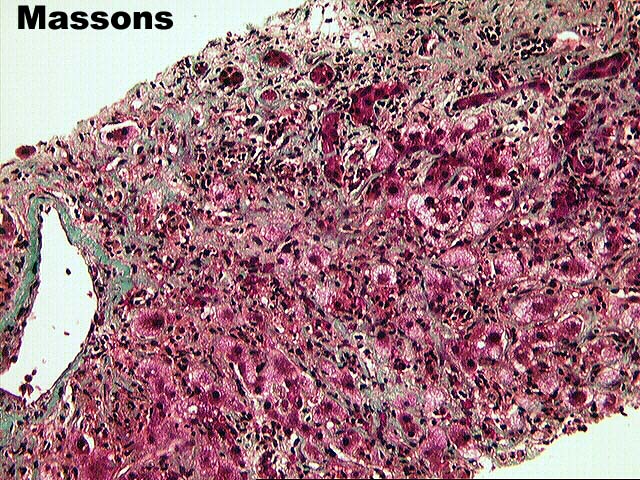
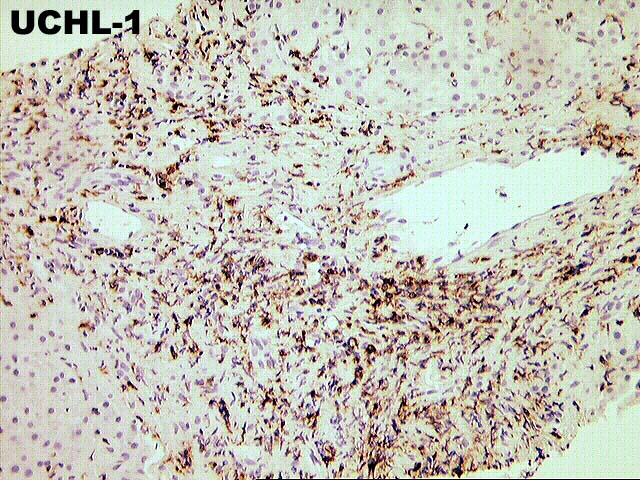
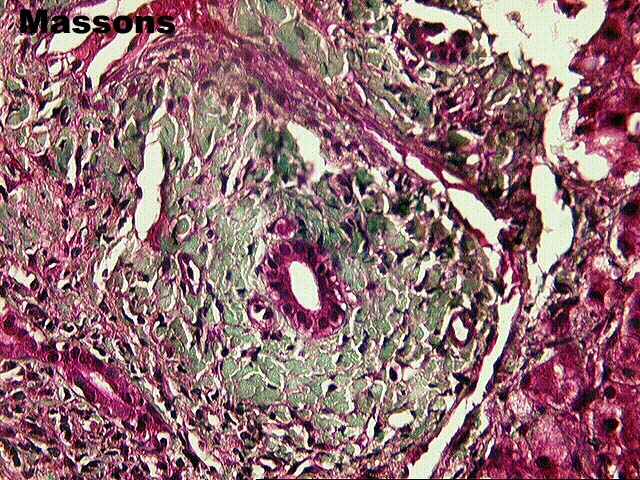
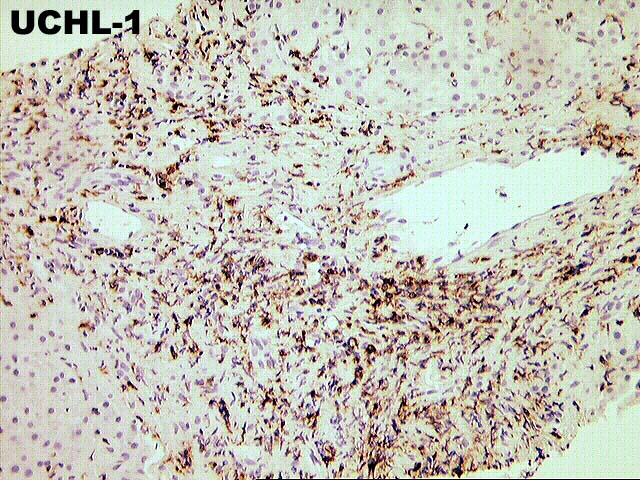
The specimen consists of one (1) HE, two
(2) EBER RNA and one (1) Masson's trichrome slide and three (3) HE, two (2)
trichrome and one (1) UCHL immunostain.
Microscopic Description - Case 10
Part 1
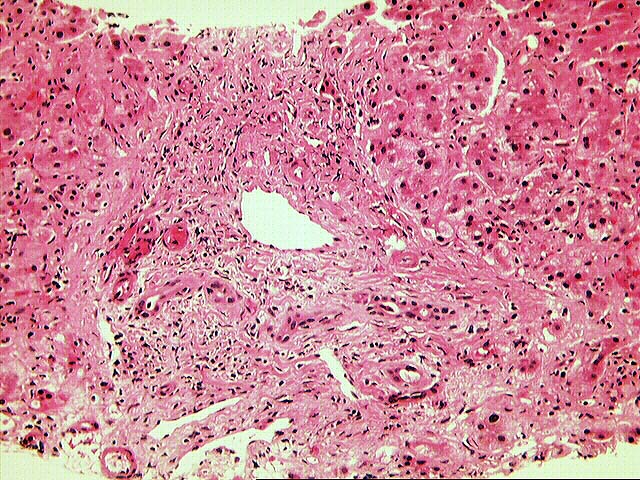
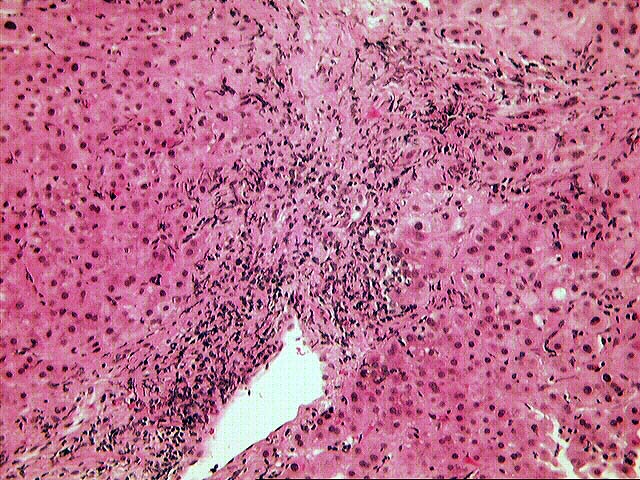
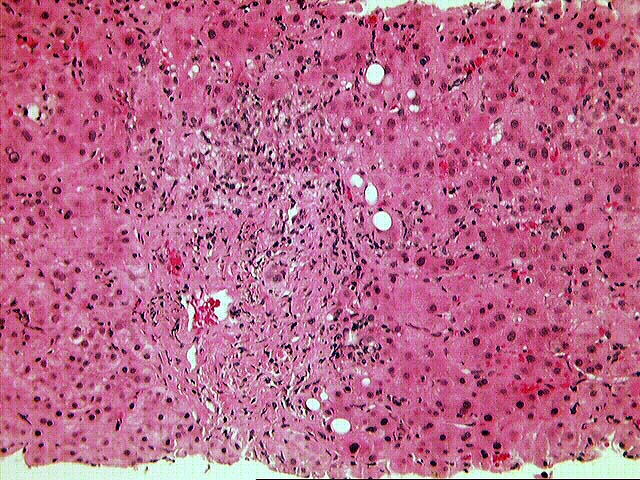
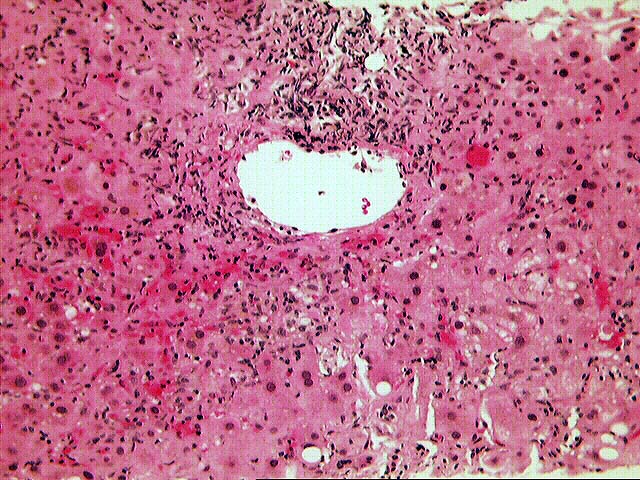
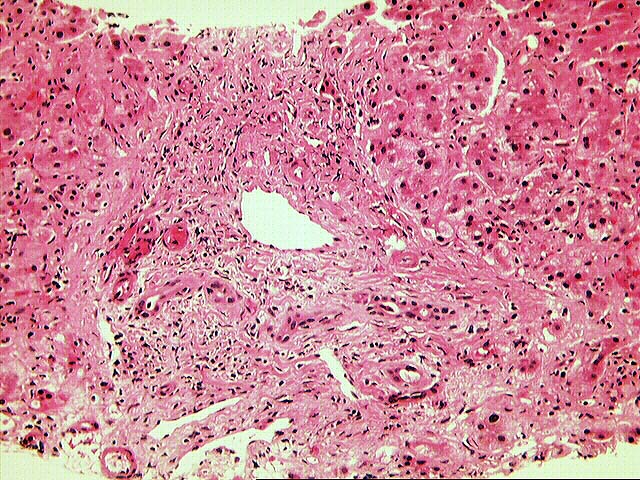
The normal lobular architecture is distorted by portal
expansion, because of fibrosis, cholangiolar proliferation and a mild to
moderate mixed inflammatory cell infiltrate. Bile duct infiltration and damage
by lymphocytes is easily seen, and there is fairly widespread atrophy and
pyknosis of the biliary epithelium. However, there is also marked interface
activity, including cholangiolar proliferation.
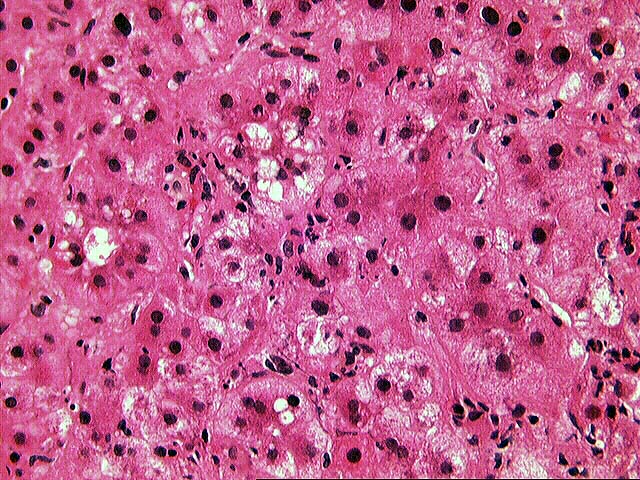
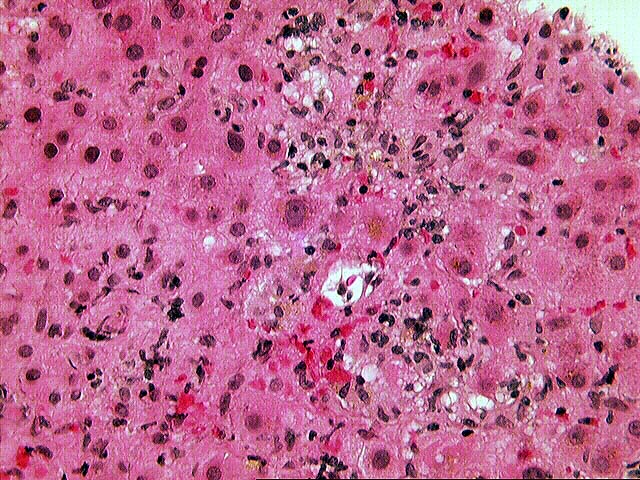
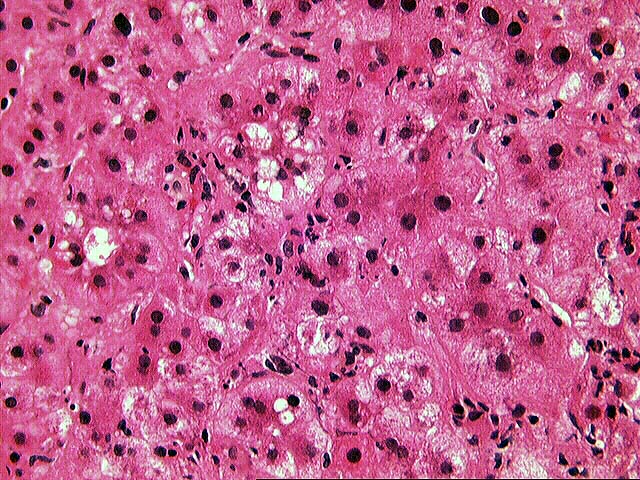
Throughout the lobules, there is moderate to severe lobular disarray, marked
Kupffer cell hypertrophy, spotty acidophilic necrosis of hepatocytes and
moderate to severe lymphohistiocytic lobular inflammation which is somewhat
accentuated in the perivenular regions. No definite ground glass cells or other
viral inclusions are detected.

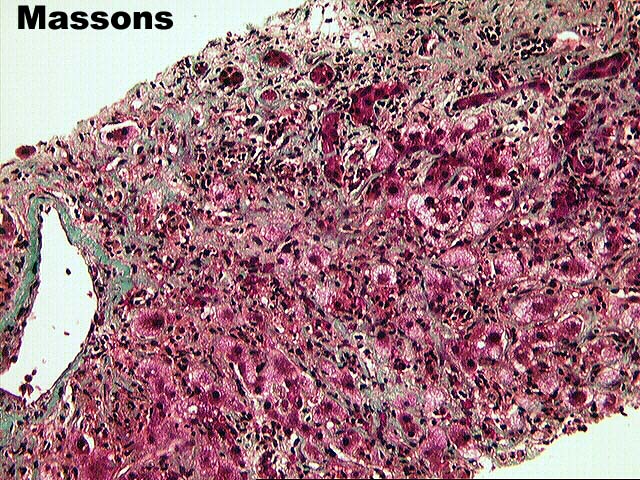
Part 2
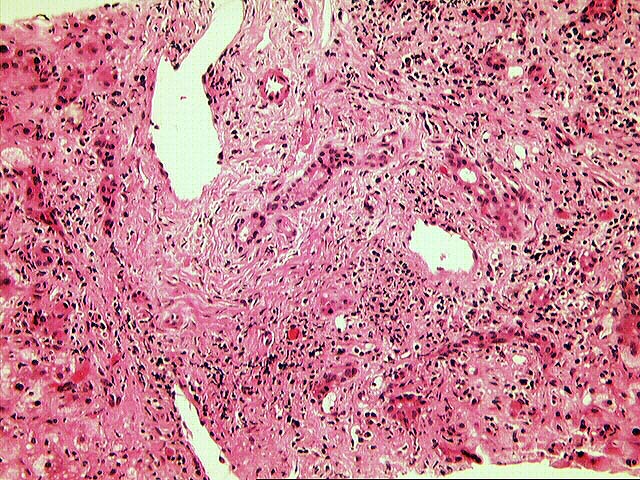
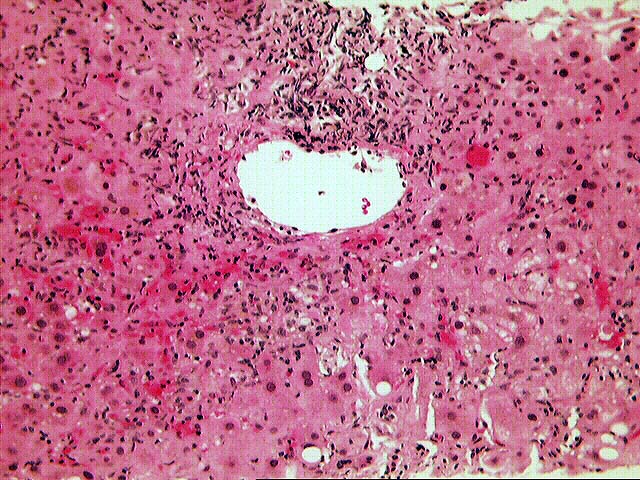
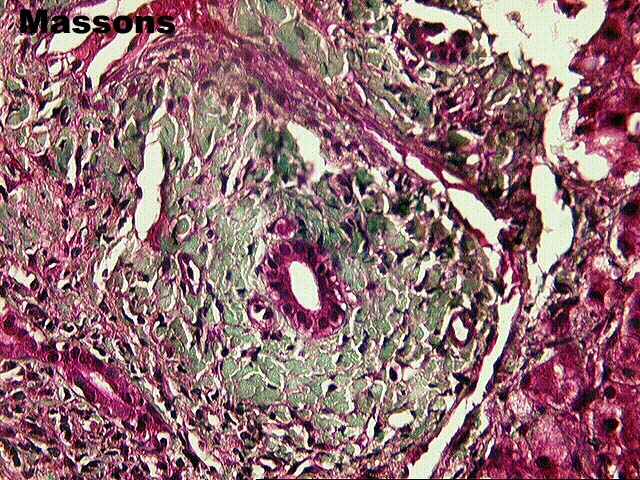
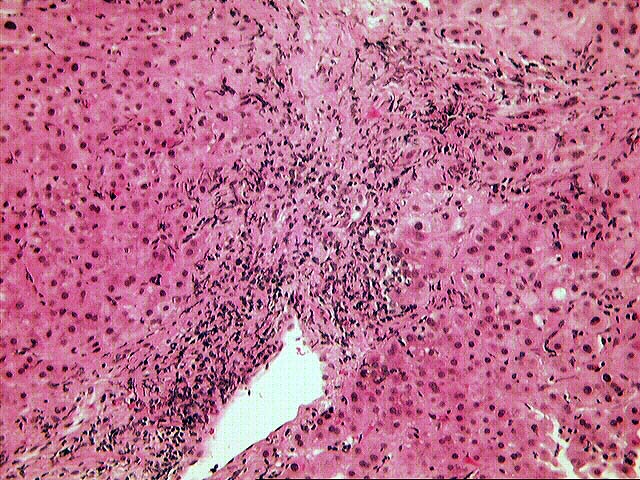
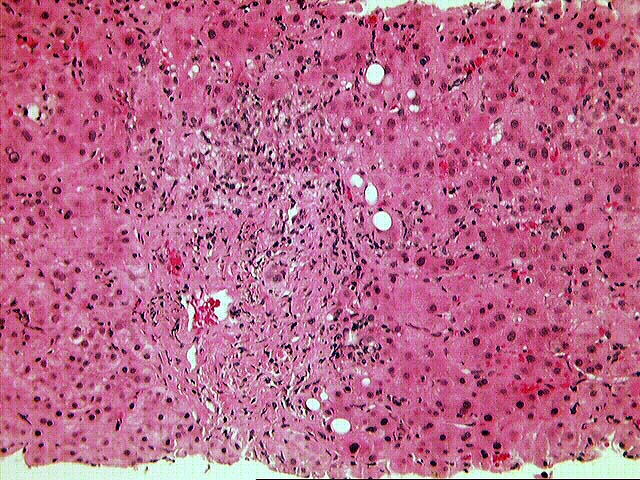
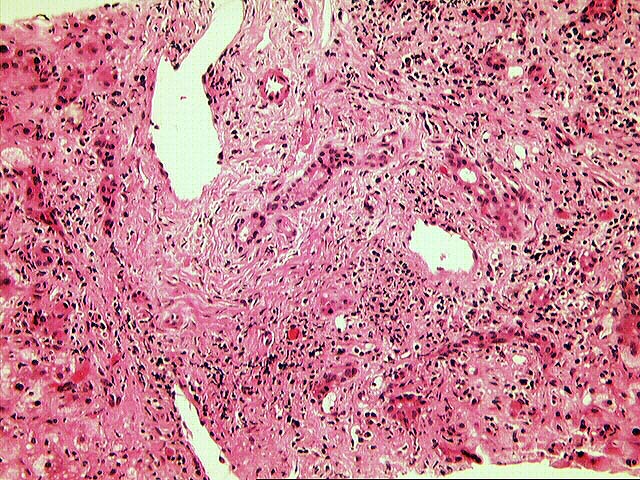
The normal lobular architecture is distorted by marked
portal expansion with focal portal-to-portal and portal-to-central bridging
fibrosis. There is also a mild, predominantly mononuclear inflammatory cell
infiltrate which is decreased somewhat in appearance to the previously biopsy.
However, there continues to be widespread bile duct atrophy and pyknosis. This
should be reflected in fairly significant elevations of the gamma
glutamyltranspeptidase and alkaline phosphatase. In addition, lymphocytic bile
duct damage is also present.
As in the previous specimen, there is mild to moderate interface activity,
including cholangiolar proliferation. Throughout the lobules, there is moderate
Kupffer cell hypertrophy, spotty acidophilic necrosis of hepatocytes,
hepatocellular swelling and lymphohistiocytic lobular inflammation which is
somewhat accentuated in the perivenular regions.
No viral inclusions or ground glass cells are seen.
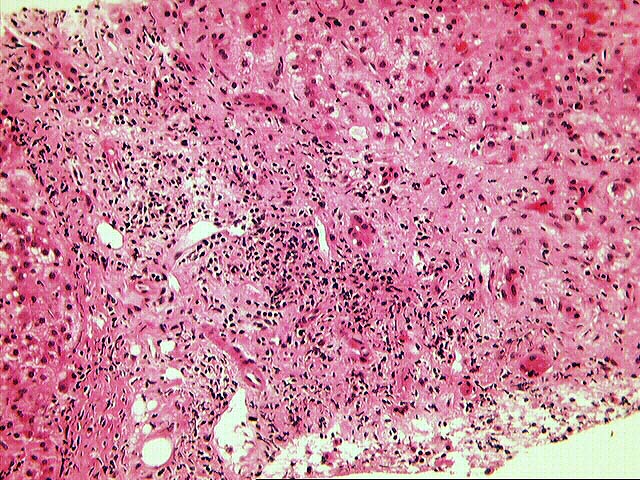
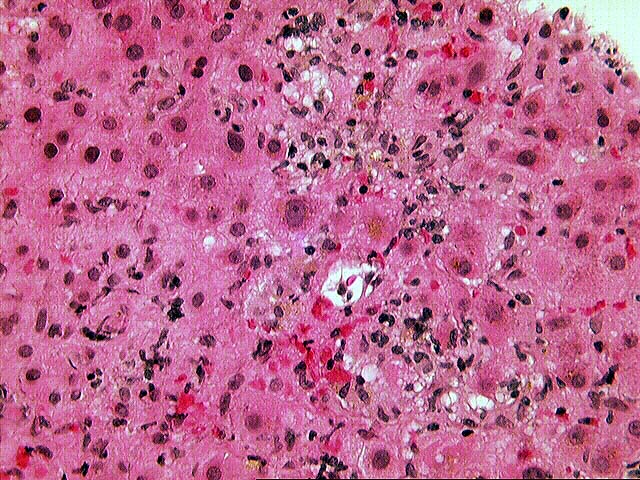
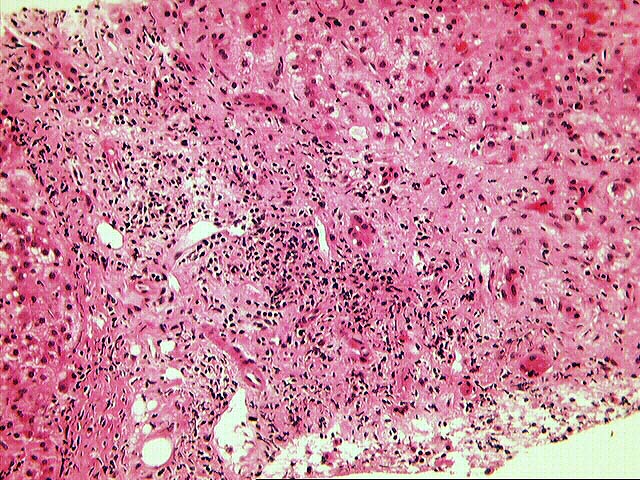
Overall, the histopathological findings in both biopsies are indicative of
more than one histopathologic insult. First and foremost, the most significant
insult appears to be an active hepatitis. This contention is based on the mild
to moderate interface activity, cholangiolar proliferation, lobular disarray,
panlobular inflammation, spotty acidophilic necrosis of hepatocytes and positive
PCR for HCV. However, a significant component of rejection is also present. In
the first biopsy, the lymphocytic infiltration and damage of small bile ducts is
far more than one would expect for hepatitis alone. In addition, there is fairly
widespread bile duct atrophy and pyknosis. The slight perivenular accentuation
of the lobular inflammation along with areas of selective perivenular fibrosis
are also more frequently seen with rejection.
Please mail comments, corrections or suggestions to the TPIS administration at the
UPMC.