Previous Biopsies on this Patient:
NONE
TPIS Related Resources:
Liver Allograft Biopsy Rejection
Criteria
Liver Transplant Topics
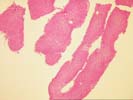
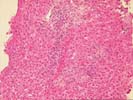
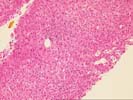
The specimen consists of a fragmented skinny needle core biopsy of liver. The basic architecture appears intact, in that the portal tracts and central veins maintain their normal spacing in most areas. There is, however, mild portal expansion because of duct, cholangiolar reactivity and possibly mild fibrosis.
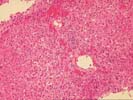
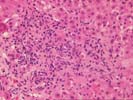
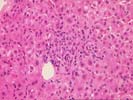
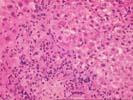
On closer examination, the triads are mildly enlarged because of cholangiolar reactivity, a mild mixed, but, in areas, predominantly acute inflammatory cell infiltrate, including an appreciable number of eosinophils. Several of the triads also contain pigmented macrophages, and several others show a loss of small bile ductules. There is mild activity at the interface zone.
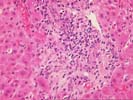
Throughout the lobules, there is Kupffer cell hypertrophy, mild disarray, and occasional acidophilic bodies. There is also an increase in sinusoidal inflammatory cells, which contain lymphocytes, neutrophils and macrophages. Again, however, eosinophils appear slightly over represented. Clusters of pigmented macrophages, suggestive of recent hepatocellular turnover and hepatocanalicular cholestasis are also seen. No definite viral inclusions are identified.
Focal areas of sinusoidal congestion are also seen.
B96-3200 (4 slides, Rhodamine Control, D/PAS, 1 Iron Control) No Rhodamine stain was received.
Sections from the skin show a mild mixed inflammation of the superficial dermal capillaries. However, no definite leukocytoclasis is seen. No involvement of the epidermis is identified. No significant increase in eosinophils is seen.
Overall, the histopathological changes are significant and indicate both acute and some chronic injury, although the latter are more mild. Even though the Rhodamine stains were reportedly negative(Rhodamine slides of sections are not received), there are some change suggestive of a "biliary" insult. This contention is based on the cholangiolar reactivity, acute inflammation and the focal loss of bile ducts. In addition, there are lobular changes are indicative of a hepatitic component.
The etiology of a combined hepatitic and biliary insult is difficult to determine from examination of the HE slides alone. In a patient with negative viral serological studies(as by history), the most likely possibilities would include, in order:
Occasional patients show overlap syndromes between autoimmune hepatitis and primary sclerosing cholangitis, although this is less likely in the face of a normal alkaline phosphatase and gamma glutamyl transpeptidase. The additional clinical history of negative AMA and ASMA along with the histopathological findings argue against the last possibility. Although it is somewhat unusual that the ANA was only transiently positive, the favorable response to corticosteroids(as per Dr. King) is in favor of an autoimmune etiology. Assay of anti-liver/kidney microsomal antibodies might be helpful.