Diagnosis comment:
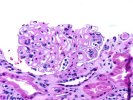
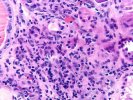
The diffuse glomerular basement membrane thickening in this case may be related to diabetes or chronic transplant glomerulopathy. However, the possibility of glomerulonephritis cannot be excluded without immunofluorescence and electron microscopic studies.
This biopsy could also be further evaluated by silver staining, and an attempt made to demonstrate spike formation as an indirect marker for the presence of subepithelial immune complex deposits.
Previous Biopsies on this Patient:
None
TPIS Related Resources:
Kidney Transplant Topics
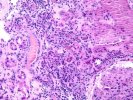
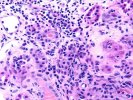
Microscopic Description
(2 H&E, 1 PAS)
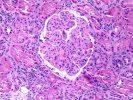
1. Glomerulosclerosis
1.1 Number of glomeruli . . . . .(35)
1.2 Number globally sclerotic . .(8)
1.3 Segmental sclerosis . . . . .( )YES(x)NO
2. Glomerulitis(g). . . . . . . . . .( )0 ( )1 (x)2 ( )3
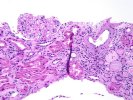
3. Interstitial inflammation(i) . . .( )0 ( )1 (x)2 ( )3
(check if present) . . . . . . .( )Neutrophils( )Eosinophils
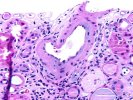
4. Intimal arteritis(v) . . . . . . .(x)0 (x)1 ( )2 ( )3
( )Not evaluable
5. Tubulitis(t) . . . . . . . . . . .( )0 ( )1 (x)2 ( )3
6. Arteriolar hyalin(ah). . . . . . .( )0 (x)1 ( )2 ( )3
( )Not evaluable
Nodular form . . . . . . . . . . .( )YES( )NO
7. Chronic glomerular change(cg). . .( )0 ( )1 ( )2 (x)3
7b. Mesangial matrix increase (mm) . .( )0 ( )1 ( )2 ( )3
8. Interstitial fibrosis(ci). . . . .( )0 ( )1 (x)2 ( )3
9. Tubular atrophy(ct). . . . . . . .( )0 ( )1 (x)2 ( )3
10. Vascular intimal sclerosis(cv) . .( )0 ( x1 ( )2 ( )3
( )Not evaluable
10b. Number of arteries with internal elastic lamina: (2)
11. Other findings:
Early changes of foamy arteriopathy with rare subendothelial lymphocytes.
12. Diagnostic categories (Check as many categories as appropriate)
( )KDARO: Normal
( )KDAB: Antibody mediated rejection
( )KDARB: Borderline change (i0-2, t0-2, v0)
(x) Acute rejection (specify g, i, t, v grades):
(x)KDAR1A: Banff Type 1A (i1-3, t2, v0)
( )KDAR1B: Banff Type 1B (i2-3, t3, v0)
( )KDAR2A: Banff Type IIA (i1-3, t0-3, v1)
( )KDAR2B: Type 2B (i1-3, t0-3, v2)
( )KDAR3: Type III (i1-3, t0-3, v3)
(x) Chronic allograft nephropathy (Specify cg, ci, ct, cv grades):
( )KDCR1a: Mild, without specific changes suggesting chronic rejection
( )KDCR1b: Mild, with specific changes suggesting chronic rejection
(x)KDCR2a: Moderate, without specific changes suggesting chronic rejection
( )KDCR2b: Moderate, with specific changes suggesting chronic rejection
( )KDCR3a: Severe, without specific changes suggesting chronic rejection
( )KDCR3b: Severe, with specific changes suggesting chronic rejection
( ) KDDR: Tubular and/or myocyte vacuolization c/w drug-associated changes.
( ) KDAT: Acute tubular necrosis.
( ) KDDO: Donor disease.
Other:
( ) Recurrent disease (specify)
( ) Subcapsular injury ( )Pyelonephritis
( ) CMV ( )PTLD
( ) Obstruction ( )Reflux
( ) Vascular thrombosis (specify)
( ) Miscellaneous