Most recently, the patient developed symptomatology that clinically was felt to possibly represent chronic rejection. Cyclosporin levels have been stable and well maintained. The patient was scheduled to be evaluated with a coronary arteriogram, however, before that study could be initiated, the patient was emergently admitted over a weekend, subsequently developing and succumbing to cardiogenic shock. Review of outside material.
Comment:
The overall change, ie, patchy fibrosis, small lymphocytic
inflammation, coronary atherosclerosis and vascular inflammation, is compatible
with an established chronic rejection process. Although the significance of
inflammatory cells within vessels is controversial, this is a recognized
component of chronic rejection and the nature of inflammation in this case
suggests that it is an extension of this process, rather than a separate acute
rejection episode event.
Previous Biopsies on this Patient:
None
TPIS Related Resources:
Heart
Allograft Rejection Grading
Heart
Transplant Topics

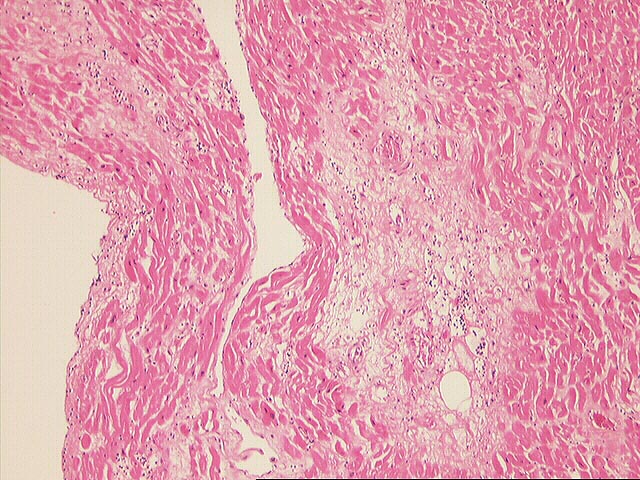

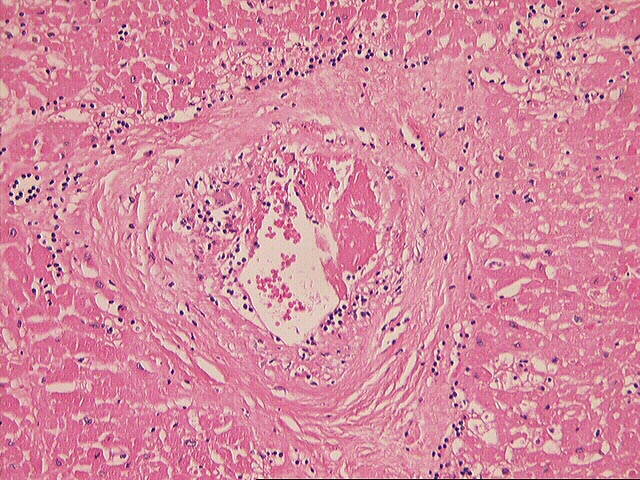
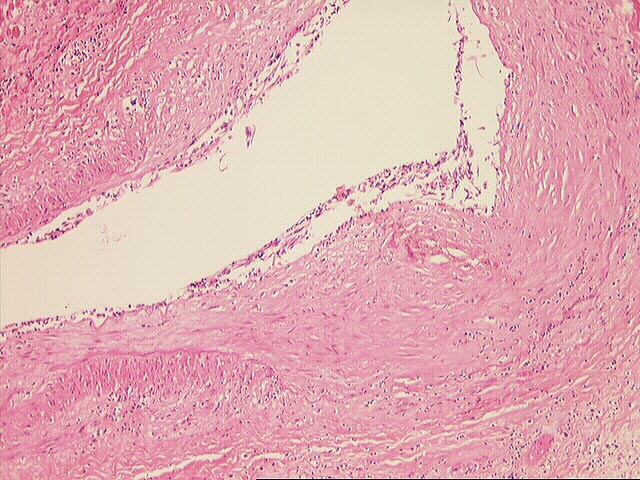
The myocardium is involved with multiple small foci of chronic inflammatory cells. These are generally well demarcated and, in some areas, are associated with areas of previous myocyte dropout. The infiltrate is predominantly perivascular and is unaccompanied by any significant eosinophilic infiltrate. Also noted is inflammation involving both intramyocardial and extramyocardial branches of coronary arteries. The latter are characterized by a circumferential intimal atherosclerotic thickening with significant numbers of chronic inflammatory cells and a moderately prominent endothelialitis. Focal thrombosis is also noted in a small intramyocardial branch. One section shows a small subendocardial infarct with mummification of myocytes.