|
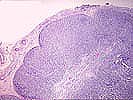
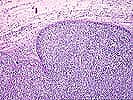
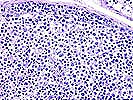

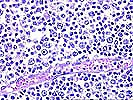
Posttransplant Lymphoid Hyperplasia. Case 1. Atypical infectious mononucleosis in a young renal transplant recipient This 3 year old boy developed cervical adenopathy 9 months after renal transplantation. There is a diffuse proliferation of mononuclear cells which respect the nodal capsule. The subcapsular sinus is patent, though it contains increased numbers of cells. Occasional small aggregates of lymphocytes suggestive of follicles are present. The proliferation is very heterogeneous due to the presence of transformed cells, in particular immunoblasts, and a background of small lymphocytes. The cell mix is evenly distributed- thus, if you were photographing this case, it would be impossible to select a field that would show a uniform population of cells, since each area contains a mix of cells. There are no large and atypical cells present. Necrosis is not a feature of this proliferation, although occasional single apoptotic cells can be seen. Additional studies showed large numbers of EBER+ cells. Immunoglobulin gene analysis and EBV terminal repeat analysis both showed a polyclonal pattern. This case is best regarded as a form of infectious mononucleosis. The histologic picture is very close to polymorphic diffuse B cell hyperplasia. However, in the latter case, there should be a more complete wipeout of the underlying architecture. In addition, since polymorphic diffuse B cell hyperplasia is usually a clonal B cell overgrowth, we might expect more plasma cells, etc. in the infiltrate. There would probably not be as many small lymphocytes, which most likely reflect the residual host T cell response in this case. However, you can see that the features overlap to some extent and a judgment as to the extent of B cell overgrowth and architectural effacement is necessary. The most decisive differential diagnosis at present is the determination of clonality, but even this is an arbitrary cutoff point. The behavior of both of these lesions is similar in that they both are normally capable of regression following reconstitution of the host immune system. This probably reflects the lack of known oncogene or tumor suppressor abnormalities in these pathologically "early" clonal overgrowths.
(Please note: Forward button takes you to photomicrographs of Case 1. When additional cases are added, it will be changed to take you to the next case) Please mail comments, corrections or suggestions to the TPIS administration at the UPMC.
If you have more questions, you can always email TPIS Administration. |
||||