The two skin biopsies are each from a different site. The biopsy from the abdomen demonstrates a relatively non-descript looking superficial perivascular dermatitis with some exocytosis and spongiosis. The referring pathologist does not see any definite keratinocyte necrosis. An occasional eosinophil is present in the dermal infiltrate. The biopsy from the arm demonstrates some very mild focal changes of a similar nature. However, the predominant finding appears to be subcutaneous vasculopathy associated with panniculitis and dermal hemorrhage.
The referring pathologist does not think this is graft versus host disease. The patient has had some intermittent diarrhea over the past few months, but this does not appear to be related. The referring pathologist feels that this could be a dermatitis component or drug reaction, but is unsure of what to call the panniculitis/hemorrhage.
Previous Biopsies on this Patient:
None
TPIS Related Resources:
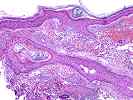

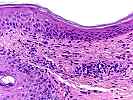
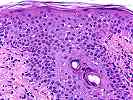
The section of the arm skin shows epidermal atrophy; very mild lymphocytic exocytosis, spongiosis and vacuolization of the epidermal basal layers; extensive solar elastosis; recent hemorrhage into the superficial dermis and focal acute inflammation of the deep dermis, which focally extends into the underlying fat. There also appears to be hemosiderin-laden macrophages scattered throughout the dermis, suggestive of previous hemorrhage into the area. No definite vasculitis is seen.
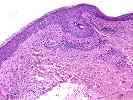
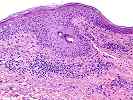
The abdominal skin shows a perivascular mononuclear infiltrate in the superficial dermis, which extends up into the epidermis, where there is marked lymphocytic exocytosis, spongiosis, satellitosis and focal keratinocyte necrosis. No definite vasculitis is seen.
Overall, given the clinical history and the histopathological findings, graft versus host disease should be given primary consideration, especially for the changes in the abdominal skin. The contention is based on the organ allograft(liver), the clinical symptoms and the histopathological findings. The presence of the recent intra-dermal hemorrhage and acute inflammation of the deep dermis and fat in the arm skin is unusual for GVHD and raises the possibility that some of the arm changes may be related to local trauma and the solar elastosis. Adverse drug reactions and viral (CMV and EBV) can at times, cause changes very similar to those seen in the abdomen. However, given the history of a recent liver transplant, history of intermittent diarrhea and the findings on biopsy, GVHD should be excluded. This can be accomplished by phenotypic analysis of the dermal infiltrate, if an appropriate HLA mismatch exists between the donor and recipient that can be recognized by monoclonal antibodies. In addition, in our experience, solid organ allograft patients with GVHD also usually have high (>2-3%) levels of donor cells circulating in the peripheral blood, and can be detected by flow cytometry. Clinical correlation with the lymphocyte phenotype, any other clinical evidence of viral infection and any temporal association of the skin changes with medications is suggested. I look forward to any follow-up in this case.