Previous Biopsies on this Patient:
None.
TPIS Related Resources:
None.
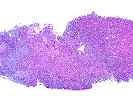
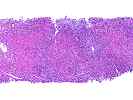
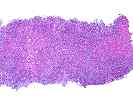
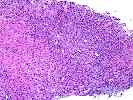
The normal lobular architecture is markedly distorted because of areas of confluent and panacinar necrosis with areas of multilobular parenchymal extinction. This appears to be occurring on the background of a relatively normal hepatic parenchyma, as in most areas, the normal spatial relationship between portal tracts and central veins is maintained, except in the areas of multiacinar necrosis.
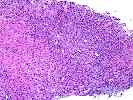
The portal tracts are expanded by prominent ductular proliferation and a mild, predominantly mononuclear, but mixed inflammatory cell infiltrate with marked cholangiolar proliferation. Proliferating cholangioles are also seen in the areas of parenchymal extinction.
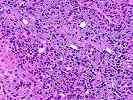
In the areas of viable hepatic parenchyma, there is hepatocellular swelling, spotty acidophilic necrosis of hepatocytes, mild steatotic change and hepatocanalicular cholestasis. No viral inclusions, ground glass cells or prominent pigment deposition are seen.
Overall, the histopathological changes are indicative of severe acute hepatitis with confluent and multi-acinar hepatocellular necrosis, bordering on submassive hepatic necrosis. This appears to be a relatively recent insult and occurring on the background of a relatively normal liver, which is consistent with the clinical history. The pattern of injury is not specific for a particular etiology, but is consistent with an adverse drug reaction and severe viral or autoimmune hepatitis, although in my experience, the severity of injury is much greater than seen with autoimmune hepatitis alone and the pattern is not typical. Nevertheless, further testing for, and consideration of autoimmune hepatitis(e.g. anit-LKM antibodies, etc.) is suggested.
Of the drugs listed, both Tegretol and Prozac, alone, have been associated with severe acute hepatitis which, in the case of Tegretol, has been occasionally fatal. Given that the insult appears relatively recent and the Prozac has been only recently added to the multi-drug regiment for epilepsy, one might be suspicious of that agent. In addition, Prozac can change the metabolism of Tegretol and increase Tegretol levels in the serum contributing to enhanced toxicity. It is not possible on the basis of morphologic findings alone to distinguish which of these two, or a combination, was responsible for the hepatic injury. However, the idiosyncratic hypersensitivity reaction to Tegretol appears to be mediated by formation of an adduct and subsequent T-cell hypersensitivity. Several groups have reported use of lymphocyte proliferation responses of peripheral blood mononuclear cells to determine if Tegretol hypersensitivity is responsible for the injury.