Laboratory tests revealed a negative serologic testing for Hepatitis C and Hepatitis B virus infection. AMA was negative at a titer of less than 1:40 and the serum gamma-globulin profile was within normal limits. Thus, there was no hypergammaglobulinemia. Antinuclear antibodies were pending at the time of discussion as well as anti-LKM antibodies.
Previous Biopsies on this Patient:
None.
TPIS Related Resources:
None.


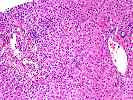
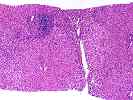


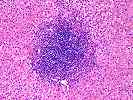
The normal lobular architecture is mildly distorted because of mild portal expansion. Approximately 10 to 15 portal tracts are identified, four or five of which show a mild to focally moderate mononuclear inflammatory cell infiltrate which is focally arranged into nodular aggregates. There is only mild focal interface activity.
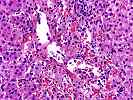
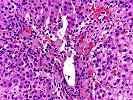
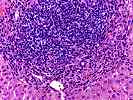
One of the most striking changes is in the lobule. There is zonal centrilobular hepatocellular dropout with congestion, focal hemorrhage and ceroid-laden macrophages. This is intermixed with a very mild infiltrate consisting mostly of small lymphocytes. No prominent plasmacytic component is identified.
Focal central-to-central bridging necrosis is identified, but no definite fibrosis is present. No prominent pigment deposition nor ground glass cells are seen. No significant increase in iron stores are seen and no large PAS/D-positive globules are identified. Overall, this difficult biopsy suggests that more than one insult may be contributing to the liver function abnormalities. First, the prominent zonal perivenular hepatocyte dropout with mild inflammation appears recent and is suggestive of a toxin or adverse drug reaction. This contention is based on the zonality of the lesion and the prevalence in most, if not all of the perivenular regions. This pattern of injury can be seen with Tylenol toxicity and numerous drugs and both a predictable and idiosyncratic hepatotoxins such as acetaminophen, halothane, other halogenated anesthetic agents, methyldopa, ketoconazole, hydralazine, as well as toxic exposure to Amanita mushrooms, carbon tetrachloride and copper sulfate.
In addition to the zonal perivenular hepatocellular dropout, there is a mild to focally moderate portal inflammatory cell infiltrate, which is focally arranged into nodular aggregates and there is mild perivenular inflammation in the areas of dropout. The inflammation present is more than one usually sees with an adverse drug reaction or hepatotoxic agent, alone. Therefore, an additional etiology should be sought. Possibilities would include an autoimmune hepatitis and chronic viral infection.
Because of the history of improving liver injury tests with conservative intervention, the negative serologic studies and the zonal centrilobular necrosis, it is tempting to attribute all of the changes to an drug adverse reaction, or interaction between a drug and alcohol given the history of illness after consuming wine. However, the inflammation seen in the biopsy is greater than the usual case, it is difficult to pinpoint a particular agent and there was about a month delay between the winery visit and the onset of jaundice. Therefore, continued workup to exclude the possibility of an autoimmune hepatitis and close clinical follow-up with serial monitoring of liver injury tests is suggested. In addition, a more sensitive testing for Hepatitis C virus infection such as HCV PCR is probably worthwhile. I look forward to more follow-up in this case.