Previous Biopsies on this Patient:
None
TPIS Related Resources:
Liver Transplant Topics
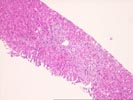
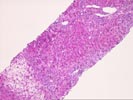
The normal lobular architecture is slightly distorted secondary to mild portal expansion because of mild fibrosis and mild duct and cholangiolar proliferation.
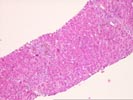
On closer examination, the triads contain a mild mixed inflammatory cell infiltrate and pigmented macrophages. Some of the epithelial cells in small bile ducts are distorted, but others are normal in appearance and, overall, bile duct distortion is not the most prominent finding. No portal venulitis is seen. Several of the triads show cholangiolar proliferation in the periportal regions with acute cholangiolitis.
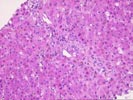
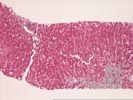
Throughout the lobules, there is panlobular hepatocanalicular cholestasis, Kupffer cell hypertrophy, and increased pigment deposition in hepatocytes and Kupffer cells, which is likely iron, considering the clinical history. There is also focal ballooning of hepatocytes and occasional acidophilic bodies. No definite ground glass cells nor viral inclusions are seen.
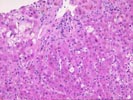
The trichrome stain reveals intact central veins in most areas. Although there is mild endothelial cell hypertrophy and very mild perivenular fibrosis in centrilobular regions, there is no significant centrilobular congestion, nor venosclerosis and thus, the changes are insufficient for a diagnosis of veno-occlusive disease.
Overall, the histopathological changes at this time are most consistent with liver dysfunction associated with sepsis. This conclusion is based on the marked cholangiolar proliferation and cholestasis, which appear to be out of proportion to the bile duct damage. Some of the mild bile duct abnormalities showing cytologic atypia might suggest a lesser component of graft versus disease, but at this time, I feel that sepsis-related liver injury is the most significant finding.