Previous Biopsies on this Patient:
None
TPIS Related Resources:
Modified Knodell Scoring
Liver Transplant Topics
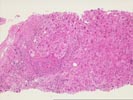
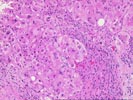
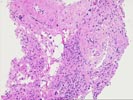
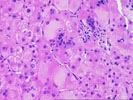
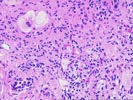
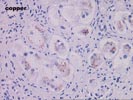
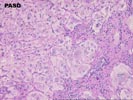
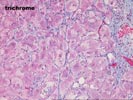
The liver biopsy shows architecture deranged by a predominantly micronodular cirrhosis with scalloped nodules of liver cells bounded by irregular fibrous bands. There is a modest, primarily mononuclear infiltrate scattered within the fibrous septa. Occasional bile ducts appear atrophic but no definite duct loss or florid duct lesions are seen. A striking features is the presence of a underlying giant cell hepatitis with numerous hepatocytes demonstrating more than four nuclei. This is a consistent feature throughout the biopsy. No ground glass hepatocytes, viral inclusions, cytoplasmic globules, or hemosiderin deposition is seen. The copper stain shows focal periportal accumulation of copper. Since other features of chronic cholestasis are not present and the liver function tests do not support a cholestatic process, this accumulation probably reflects the nonspecific depositon that can be seen in many forms of chronic liver disease.
Postinfantile giant cell hepatitis is a clinicopathologic entity that is not well described in the literature. Although some cases have known cause (including hepatitis viruses and drugs), many instances are associated with various autoimmune features including positive ANA and hemolytic anemias. Typically the pateints suffer a slowly progressive course, although immunosuppressive therapy has sometimes yielded a response. We have noted several cases that have recurred following liver transplantation. Thank you for sending this fascinating case. I would appreciate any follow-up information you receive.