Previous Biopsies on this Patient:
None
TPIS Related Resources:
Liver
Allograft Rejection Grading
Liver
Transplant Topics
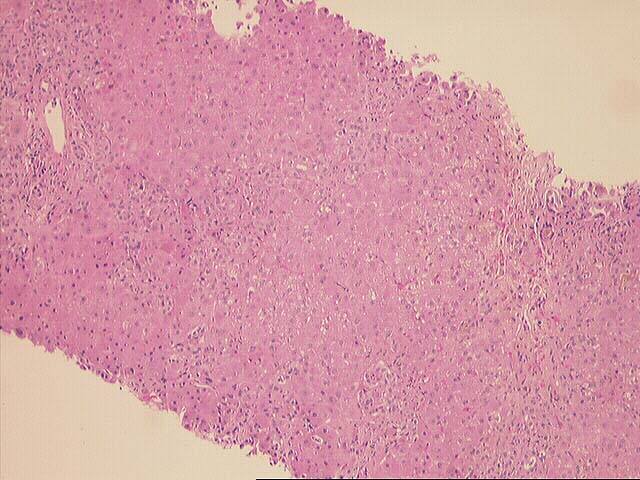
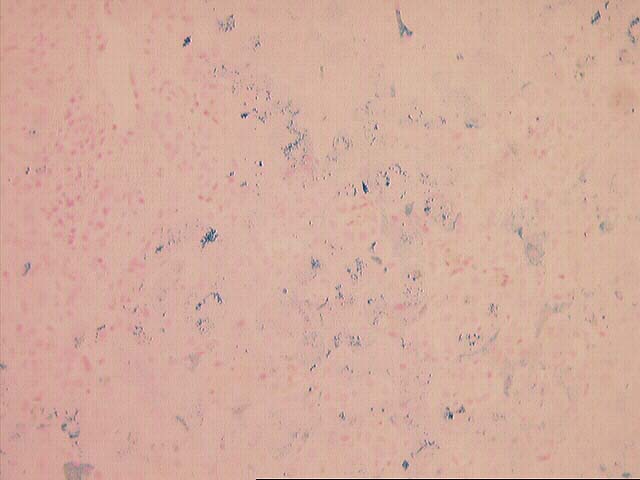
The normal lobular architecture is distorted by marked portal expansion with focal portal-to-portal bridging. The triads are expanded because of duct and cholangiolar proliferation along with fibrosis. There is no significant portal inflammatory cell infiltrate, and no duct damage or venulitis are seen. One small portal vein shows an organizing thrombus.
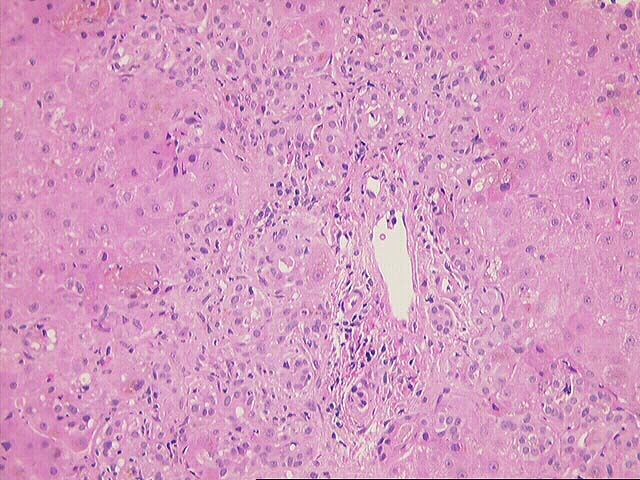
There is marked cholangiolar proliferation in the interface zone and cholangiolar bile plugs are seen.
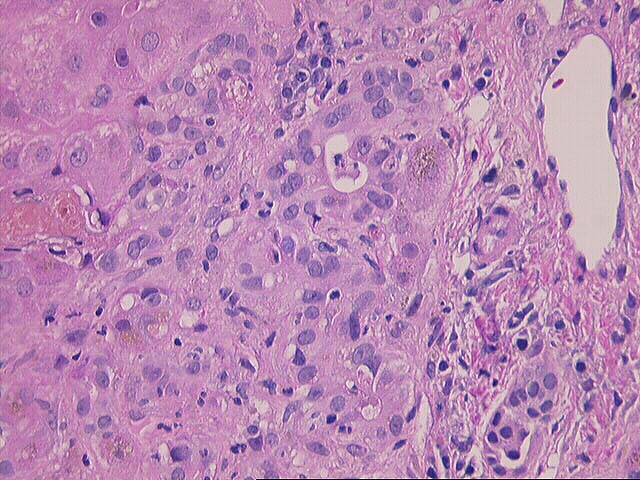
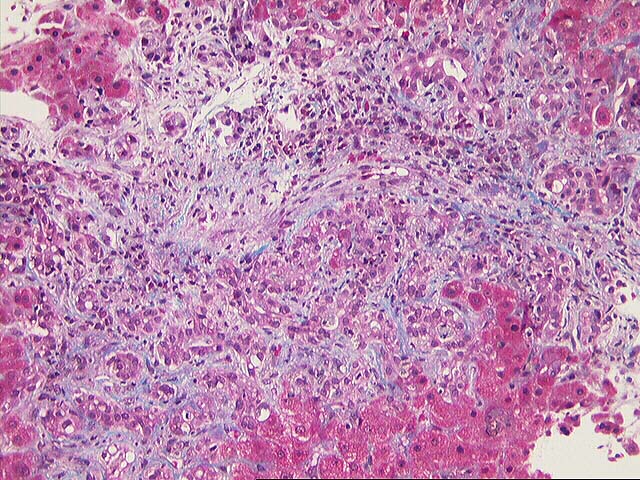
Throughout the lobule, there is marked Kupffer cell hypertrophy, enlarged hepatocytes with large eosinophilic nucleoli and panlobular hepatocanalicular cholestasis. Pseudorosetting of hepatocytes is also seen. One cell is suspicious for ground glass change which should be investigated with the use of immunohistochemical studies for Hepatitis B core and surface antigens.
Overall, the histopathological changes are most consistent with a severe preservation injury and/or sepsis, which is consistent with the clinical history. No evidence of acute or chronic rejection is seen.