PART 2: ALLOGRAFT LIVER, NEEDLE BIOPSY (1/21/97) -
PART 3: ALLOGRAFT LIVER, WEDGE AND NEEDLE BIOPSY (2/6/97) -
COMMENT:
Although significant bile duct loss is not noted, the changes of
chronic duct injury raise the possibility of early chronic
rejection. In some instances, similar duct changes can be
associated with chronic hepatitis C, but they are typically
focally distributed in that setting. Correlation with liver
enzymes (including the GGTP) is necessary.
Previous Biopsies on this Patient:
NONE
TPIS Related Resources:
Liver Allograft Rejection Grading
Liver Transplant Topics
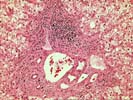
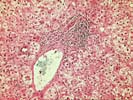

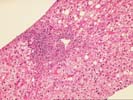
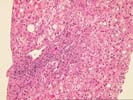
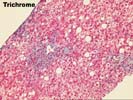
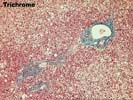
The liver biopsy show progression of chronic hepatitis with the appearance of features suggestive of chronic hepatitis C. There is portal fibrosis and mild inflammatory activity in the initial biopsy together with minimal macrovesicular steatosis. These changes become more pronounced in the second biopsy where early portal to portal bridging fibrosis is identified. Here the inflammatory activity is mild but there is an occasional lymphoid aggregate and mild macrovesicular steatosis, features consistent with chronic hepatis C. In this biopsy occasional sporadic bile ducts appear atrophic and have enlarged darkly staining nuclei. These changes more evident in the final biopsy which demonstrates several angular and dysmorphic duct with densely staining cytoplasm. Because of there uniform distribution in the latter biopsy the possibility of chronic rejection needs to be considered in addition to chronic hepatitis C. Clinical correlation with the gamma glydanile transpeptidase levels would be helpful in further accessing the bile duct injury.