COMMENT:
Among the etiologic considerations are alcohol abuse, obesity, diabetes, certain drugs, and a variety of other less common conditions. The cause of the granulomas is not evident, but sarcoidosis should be excluded on clinical grounds; no evidence for primary biliary cirrhosis, infectious causes, or drug-induced granulomas is noted.
Previous Biopsies on this Patient:
NONE
TPIS Related Resources:
Liver Allograft Biopsy Rejection
Criteria
Liver Transplant Topics
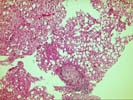
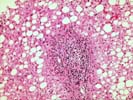
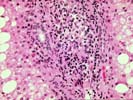
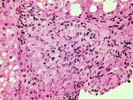
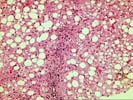
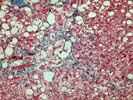
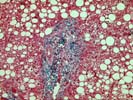
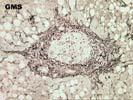
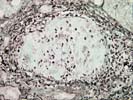
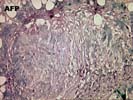
The liver biopsy shows intact hepatic architecture, but there is mild pericellular fibrosis. Moderate steatosis is present and is characterized by both macronodular steatosis and a minor component of micronodular steatosis. Occasional hepatocytes show cytoplasmic lucency and swelling associated with cytoplasmic clumping. Although no classic Mallory bodies are seen, the presence of pericellular fibrosis and sparse inflammation in these areas suggest a mild, low-grade steatohepatitis. In addition, there are scattered well-formed epithelioid granulomas, which are associated with peripheral rims of fibrosis and occur within both lobules and portal tracts. In general, hepatic granulomas can have a large number of causes, but most cases in which a cause can be specifically identified fall into several groups. Primary biliary cirrhosis is one such possibility, but other histologic features and the clinical findings do not support this diagnosis. Sarcoidosis remains a consideration because of the fibrosis noted with the granulomas; this diangosis should be explored on clinical grounds. Many drug-induced hepatic granulomatous reactions tend to have less well-formed granulomas that develop in a hepatitic or cholestatic background, neither of which is seen in this case. In addition, review of the extensive list of drugs the patient is taking shows none that have been associated with granulomas. Finally, infectious causes need to be excluded; the AFB and GMS stains provided show no organisms. In our experience, if none of these four general categories apply, the cause of the granulomas usually remain somewhat of an enigma. Thank you for sending this challenging case. I appreciate any follow-up information you received.